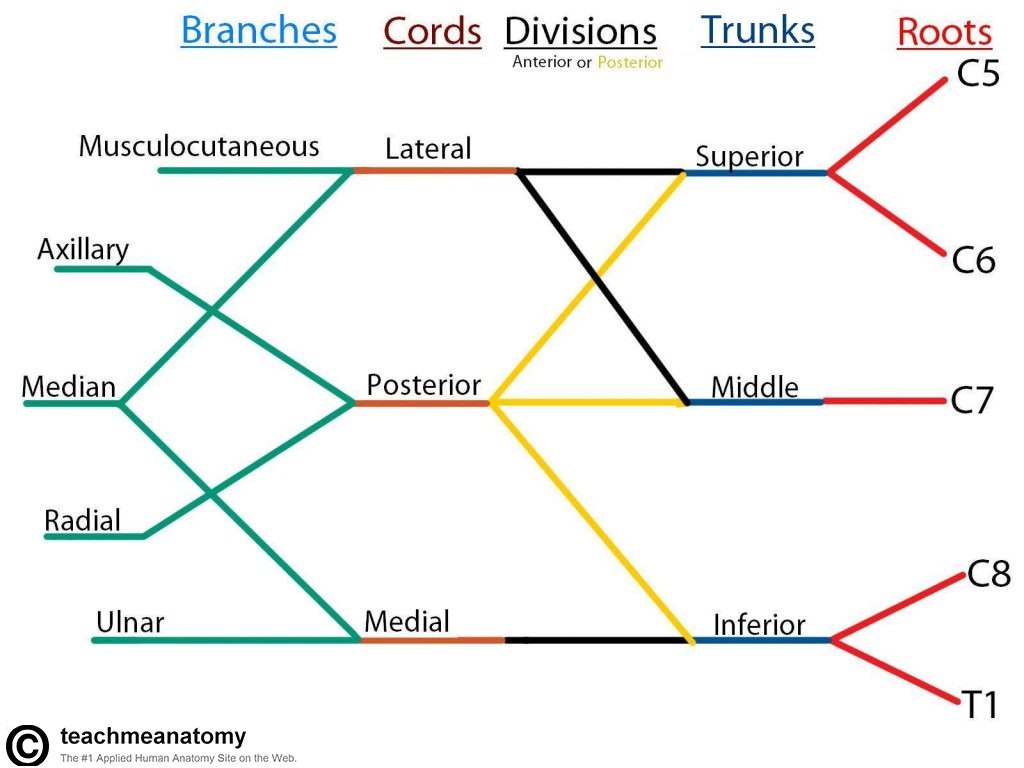
Upper extremity nerve blocks involve blocking the brachial plexus at different points – the major blocks are interscalene, supraclavicular, infraclavicular, and axillary. So how do we decide which blocks are appropriate for a given surgery? What are the pros/cons of certain blocks over others? First of all, let’s start with a diagram of the brachial plexus.
SHOULDER SURGERY
Interscalene block (targets brachial plexus roots)
- Excellent coverage (shoulder, upper arm, elbow) with potential for successful catheter placement.
- Very low risk for pneumothorax or vascular injury.
- Phrenic nerve palsy is common – ~100% with nerve stimulator placement, very low risk with ultrasound guidance.
- Possible to develop Horner’s syndrome as well as laryngeal nerve palsy.
- Ulnar nerve distribution is often spared.
Supraclavicular block (targets trunks and proximal divisions)
- Very good coverage but poor candidate for catheter placement
- Phrenic nerve palsy risk somewhat less (50% with nerve stimulator, very low with ultrasound)
- Higher risk for pneumothorax
- Ulnar nerve missed ~10% of the time.
For shoulder surgeries (arthroscopies, rotator cuffs, etc.), I’ve been sticking to interscalene blocks due to their excellent coverage and reliable placement of catheters. Due to diaphragmatic compromise from phrenic nerve palsies, this may be a poor choice in patients with low pulmonary reserves (ie, COPD).
MID-HUMERUS TO HAND SURGERY
Infraclavicular (targets cords)
- Landmarks are often difficult to identify and block is technically challenging to place
- Very reliable catheter placement and fantastic coverage of forearm, wrist, and hand
Axillary (targets terminal branches)
- Patchy block which often misses musculocutaneous nerve
- Cannot reliably place catheter
A well-placed infraclavicular block is priceless! While they are more difficult to place, I’m becoming more proficient at identifying the landmarks and using ultrasonography to carefully guide the needle to the lateral, medial, and posterior cord targets (“triple injection”). An axillary block is easily to place blindly (palpate the axillary artery and inject adjacent to it), but it’s patchiness and lack of musculocutaneous nerve coverage make it less reliable.
As a side note, the intercostobrachial nerve (branch of T2, so not part of the brachial plexus) innervates the medial aspect of the upper arm and usually needs to be blocked if the surgeon is using a tourniquet. This is achieved by placing a field block using a long skin wheal 3 cm medially from the axilla.





