Heparin is a naturally occurring, negatively charged carbohydrate consisting of molecules with different lengths (unfractionated). It potentiates the activity of antithrombin (AT) III which inactivates thrombin and factor Xa based on the size of the heparin molecule. Fractionated, low molecular weight forms of heparin (ie, enoxaparin) are more selective for factor Xa inhibition.
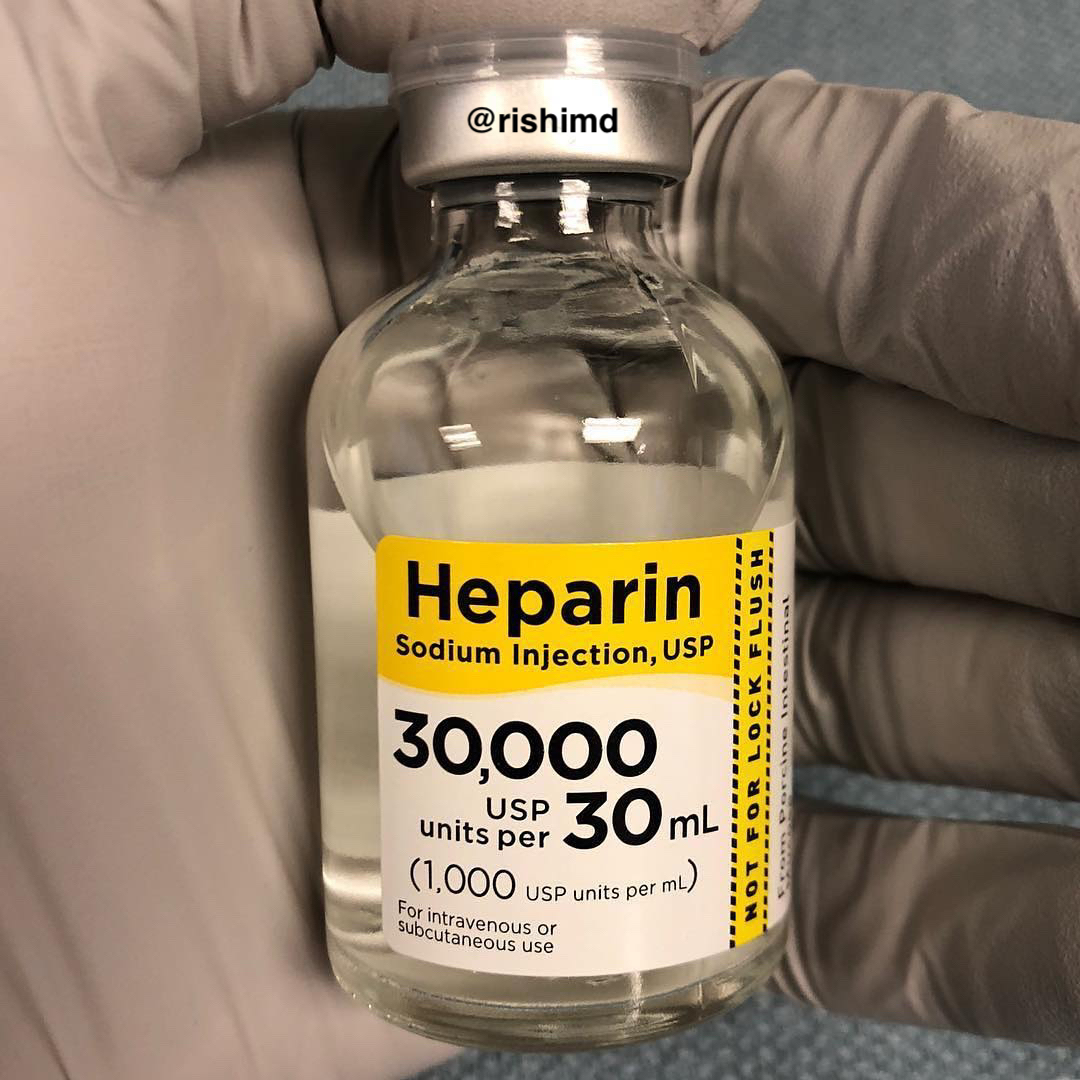
In the cardiac ORs, large amounts of heparin (10,000 – 30,000 units, remember 1 mg = 100 units) are administered prior to cardiopulmonary bypass (CPB). Due to a disruption of angiotensin II endothelial signaling, hypotension may result after a large bolus. We measure heparin’s efficacy through activated clotting time (ACT) and heparin levels which also help determine how much reversal (protamine) to administer post-CPB. Heparin is arguably the most important medication in cardiac anesthesia.
As an intensivist, I most commonly use heparin for patients on mechanical circulatory support (ie, ECMO, Impella, IABP), as pharmacologic prophylaxis against venous thromboembolism (VTE), and as anticoagulation for DVT/PE and atrial fibrillation.
Heparin induced thrombocytopenia (HIT) is an immune-mediated degradation of platelets I screen for clinically, using the “4T Score” (degree of thrombocytopenia, thrombosis, timing, and other possible etiologies) and serologic/function testing with anti-PF4 antibodies (low specificity) and serotonin release array (only a few places run SRAs). If I’m concerned about HIT, I’m switching heparin to bivalirudin or argatroban.
Drop me a comment below with questions! 🙂






What labs are you tracking to monitor Bivalirudin? How often and what your goal coag?
Hey Gina! I still use ACT intraoperatively (roughly every 30 minutes). Coagulation goals depend on the type of case I’m doing.