Let’s review what a complete operating room anesthesia set up entails using the well known “MSMAIDS” mnemonic.
MSMAIDS stands for machine, suction, monitors, airway, IV, drugs, and special.
MACHINE
- Start the anesthesia machine, monitors, and computer
- Run the self-test
- Adjust the machine parameters depending on your case (general anesthesia, MAC) and patient’s information (age, ideal body weight)
- Check the volatile agent levels
- Between cases, the most important self-test is the low-circuit pressure test. To do this, we occlude the Y-piece, close the pop-off valve, flush O2, and ensure that there’s no pressure leak up to 40 cm H2O. I also like to switch on the ventilator just to see if it works.
- Make sure there’s an AmbuBag (bag-valve mask) in the room!
SUCTION
- Make sure the suction circuit is connected and that a Yankauer suction tip is available. Most of the time you’ll also need to get a OG tube prepped with lubrication to evacuate the gastric contents prior to a general anesthetic.
- I usually switch the suction off at this point but make sure it’s readily available.
MONITORS
- Outside of the machine’s internal monitors (O2 analyzer, etc), you’ll need a plethora of external monitoring devices.
- EKG leads, pulse oximeter, temperature probe (esophageal stethoscope, Foley, skin probe), blood pressure cuff
- Depending on the nature and duration of the case, you may need a transesophageal echo (TEE), arterial/central line set up, BIS monitor, cardiac output monitor, or something entirely new. Anesthesia techs are extremely helpful in setting these up!
AIRWAY
- Standard or reinforced endotracheal tube (ETT) with stylette placed and cuff checked for a leak
- Laryngoscope of your choice – I’ve been using the Mac 4 recently. Make sure the light is functional.
- Oral airways
- Make sure laryngeal mask airways (LMAs), bougies, and Glidescope/C-Mac are readily available in the event of a difficult airway
IV ACCESS
- I usually do this after the room is set up. Most of my patients start with a 20 gauge peripheral IV (PIV) for anesthesia induction. If I need more lines, I put them in after they’re asleep. 🙂
- This is also when I decide whether the patient needs a pre-induction arterial line. Otherwise, it goes in after intubation.
MEDICATIONS (a few examples)
- Pre-medication: fentanyl, midazolam, Pepcid, Reglan, Bicitra
- Induction: propofol, etomidate, rocuronium, succinylcholine, lidocaine, Nimbex
- Volatiles: sevoflurane, isoflurane, desflurane
- Pressors: phenylephrine, norepinephrine, ephedrine
- “Downers”: nitroglycerine, esmolol
- Analgesics: Toradol, morphine, fentanyl, hydromorphone, Tylenol
- Antibiotics: cefazolin, cefepime, vancomycin, etc
- Reversal: neostigmine, glycopyrrolate
- Other: Zofran, dexamethasone
SPECIAL
- The obligatory “catch all” category. This is for everything else: OG/NG tubes, Bair Hugger blanket, fluid warmer, etc.
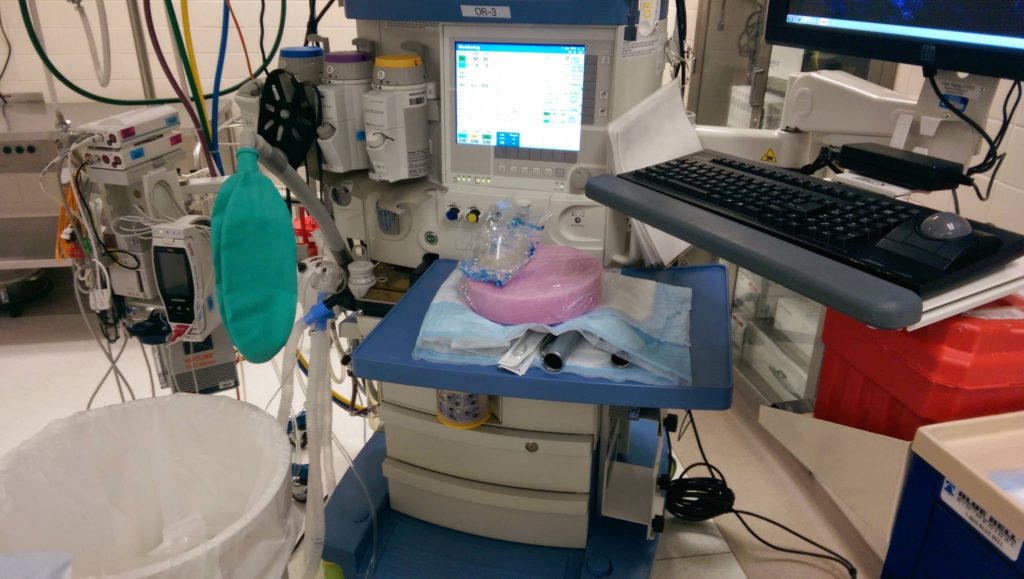
Now here are two images comparing my set up at two different hospitals. Notice the similarities and differences.







It’s is veryuseful to us
You must assure that the backup O2 cylinder on the back/side of the anes machine is not empty; it must be checked by turning the valve which also ascertains that a wrench is available to turn it on if needed.
Do you allow your OR housekeepers to set up a anesthesia machine with the suction canisters, Yankauer suction tips, ambu bags, face masks and airway tubing??? Do you feel it’s the responsibility of the housekeeper? Just curious. Thank you!
Depending on the hospital, anesthesia technicians are tremendously helpful in facilitating room turnover including setting up the basic items you mentioned; however, I’ve also rotated at hospitals where we’re responsible for everything. I don’t think it’s the responsibility of the housekeeper. The provider should be able to do this on his/her own.