One of the most essential skills of airway management is the ability to bag ventilate a patient. This can be a reassuring sign in the event of an otherwise difficult airway and is something to fall back on if intubation is unsuccessful. That being said, most people don’t want to bag ventilate for hours, so at some point laryngoscopy with intubation is performed. Here are some basic considerations for ventilation and intubation.
BEFORE INTUBATION
- Position the patient to optimize airway anatomy
- Adjust the table height so the patient’s head is at your xiphoid.
- Place in sniffing position
- For obese patients, try to position the external auditory meatus at the same level as the sternal notch.
- Mask ventilation tomaintain oxygenation and ventilation
- Place the mask along the bridge of the nose and roll down over the mouth.
- Create a ‘C’-shape between your thumb and index finger. Place the middle and ring fingers along the mandible with your pinky on the angle of the mandible.
- Elevate and jaw thrust the patient’s face to the mask. Most of the force should bring the mandible up to the mask.
- If unable to move air, insert an oral airway (start in reverse orientation and spin it into position) and resume mask ventilation.
- If still unsuccessful, proceed to two-hand ventilation with your thumbs on either side of the mask and the remaining fingers along both sides of the mandible.
- Proceed to direct laryngoscopy (DL) – if unable to ventilate or intubate, call for help and/or place a laryngeal mask airway (LMA).
DIRECT LARYNGOSCOPY
- Protect the patient’s eyes and remove everything from the airway (oral airway, mask).
- Scissor the mouth open strongly with your right thumb and forefinger. Make sure the tongue and lips are clear of the teeth.
- Insert the laryngoscope blade (held in the left hand) from the right side and sweep the patient’s tongue to the left. Verbalize everything you are seeing.
- Do NOT tilt the blade backward as this can inadvertently damage the teeth and/or lower lip.
- Pass the styleted endotracheal tube passed the vocal cords, remove the stylet, inflate the cuff (palpate the pilot balloon to confirm a good seal), and attach the anesthesia circuit.
- Confirm equal, bilateral breath sounds and end tidal CO2 return. Turn on the volatile agent, place the patient on the ventilator, and let the magic happen! 🙂
OTHER
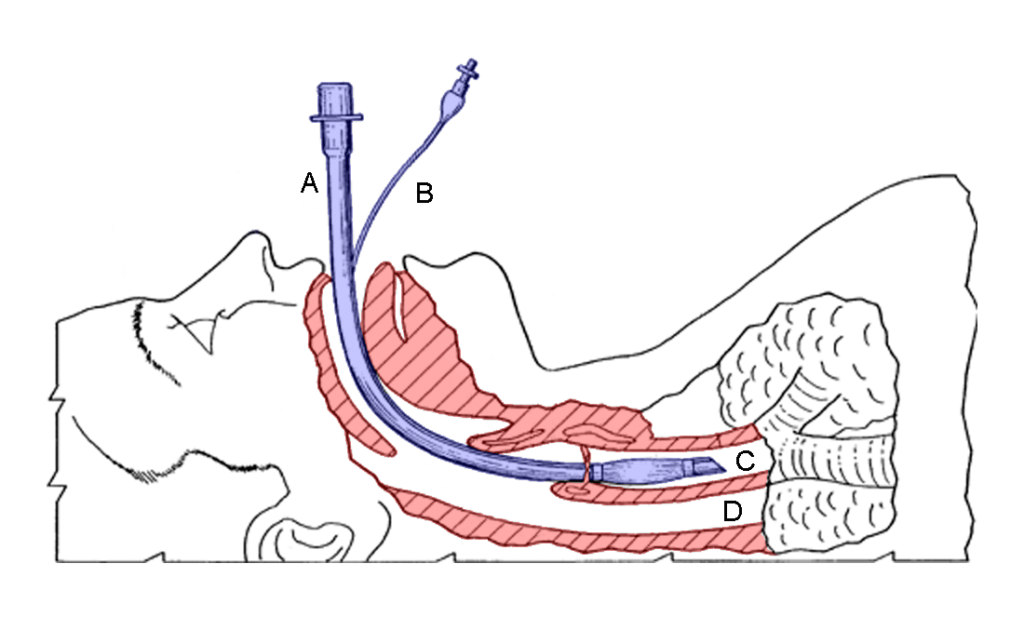
- Laryngeal mask airway (LMA)
- Often used as a rescue device in the “can’t intubate, can’t ventilate” scenario.
- Fully deflate the LMA reservoir and apply a lubricant to the posterior surface.
- Slide the LMA along the hard palate so it follows the natural curvature into the posterior oropharynx.
- Inflate the seal, attempt to mask ventilate the patient, and ensure tidal volumes and airway pressures are adequate.
- Make sure the patient is “deep” before beginning surgery.
- When removing the LMA, do NOT deflate the cuff. This allows the LMA to sweep out secretions as it exits.
- Bougie-aided intubation
- The bougie is a long, thin plastic tube with slight distal flexion useful in higher grade views.
- Once in the trachea, the distal portion can hit the anterior cartilaginous tracheal rings – you’ll feel the tip knocking against these rings on the way down to the carina where you’ll meet resistance. If the tip flips and travels along the membranous trachea, you won’t feel the characteristic knocking.
- The endotracheal tube can then be threaded over the bougie.
- Fiberoptic intubations can be used for awake or asleep intubations.
- Glidescope and C-Mac are video laryngoscopes useful for higher grade airways.