This post outlines the steps in traditional, central cannulation for cardiopulmonary bypass (CPB). Depending on the nature of the surgery and the patient’s comorbidities, other sites are often cannulated (left heart bypass, femoral-femoral peripheral cannulation, etc.)
Cardiothoracic surgery is a complex art requiring precision and coordination among various teams. To facilitate surgery, CPB allows the surgeons to have a bloodless, motionless field to operate in. The lungs and heart are both arrested, while the CPB circuit handles systemic perfusion and gas exchange.
Once our surgical colleagues are ready to begin CPB cannulation, cardiothoracic anesthesiologists will work with perfusionists to administer systemic heparinization. This is usually 300-400 units/kg targeting an activated clotting time (ACT) of greater than 450 seconds. This ACT target varies at each institution and is sometimes combined with a heparin level assay. Heparin is arguably the most important drug in cardiac anesthesia. Whenever I heparinize, I ensure that the medication goes through my most reliable access (i.e., a central line that I can aspirate blood from). If we were to expose the patient to the CPB circuit without heparinization, the pump and oxygenator would clot, leading to a catastrophic outcome. As a side note, heparin boluses tend to decrease ionized calcium resulting in transient vasodilation and hypotension. Nothing a small bolus of norepinephrine can’t fix. 😉
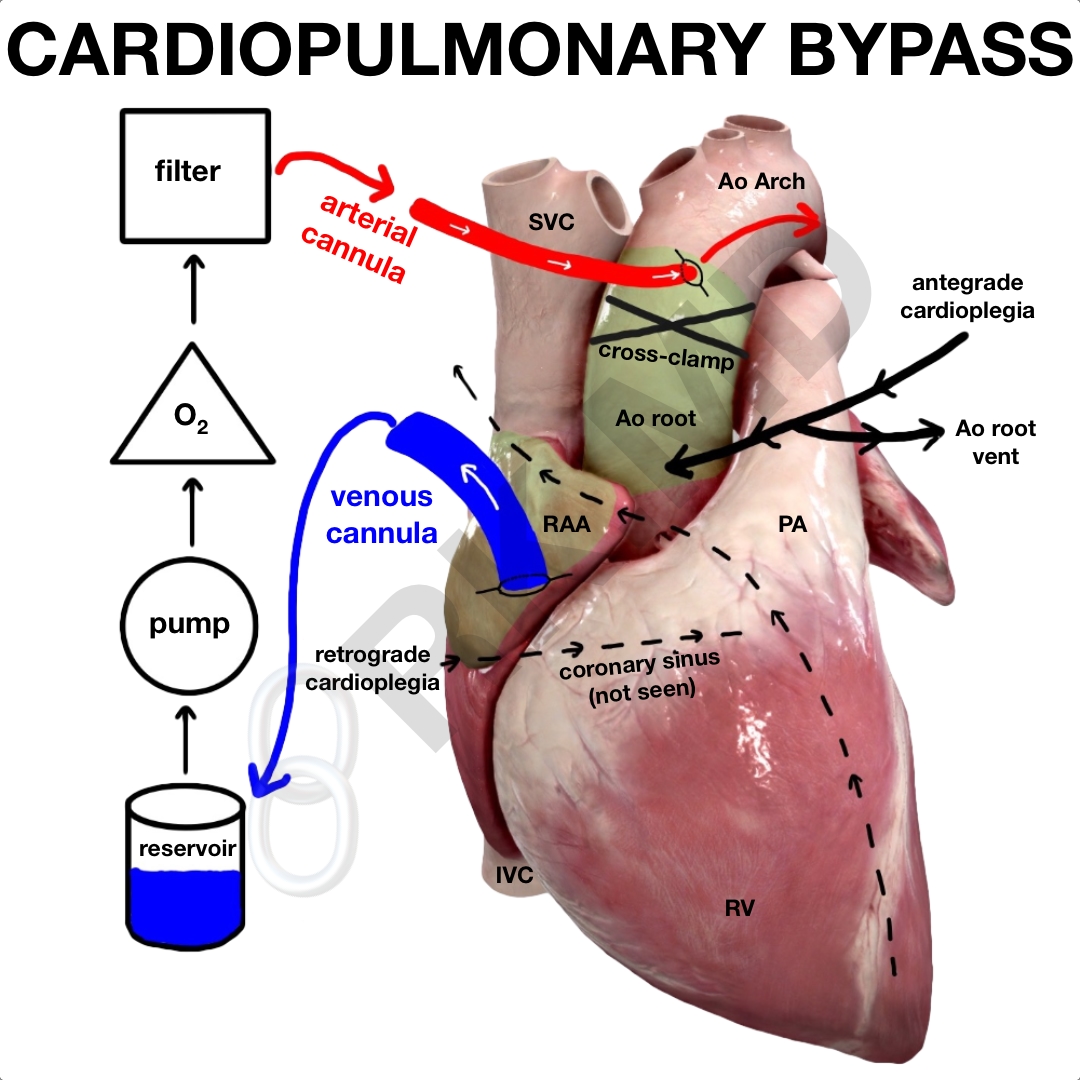
BASIC CPB CIRCUIT
The CPB circuit drains blood from the venous cannula into a reservoir, usually by gravity or vacuum suction, runs it through a pump (centrifugal is more popular than roller pumps these days) and then to an oxygenator where gas exchange occurs, and halogenated volatiles like isoflurane are added. Finally, the blood passes through an arterial filter on its way back to the body through the arterial cannula.
ARTERIAL AND VENOUS CANNULATION
The surgeons begin cannulation by placing one or two concentric purse-string sutures on the anterior surface of the ascending aorta (Ao) for the smaller arterial cannula and on the right atrial appendage (RAA) to access the right atrium (RA) and inferior vena cava (IVC) for the larger venous cannula. Once the sutures are in, and the ACT is at goal, the aorta is cannulated first. We want to get the systolic blood pressure down to ~100 mmHg to avoid creating a dissection flap during aortic cannulation. Next, an aortotomy is performed through the purse-string sutures. The cannula is directed upwards into the aortic arch. The purse strings are cinched down to tighten the opening around the cannula. This same process is repeated for the venous cannula in the RAA.
Once CPB is initiated, an aortic cross-clamp is placed between the aortic cannula and the antegrade cardioplegia cannula. At this point, the heart is still beating until cardioplegia is administered. We can also stop ventilating the patient’s lungs as the CPB circuit will handle gas exchange.
Why is the aorta cannulated first? With an arterial cannula, it’s possible to crash onto CPB in the event of hemodynamic instability immediately. The venous cannula basically supplies “fuel” for the CPB circuit; however, in the short term, volume can be directly added to the reservoir in the form of crystalloid, blood, albumin, FFP, etc. When decannulating, the aortic cannula is also the last removed to allow transfusion of remaining blood within the CPB circuit into the patient and insurance if the patient needs to crash back on CPB.
CARDIOPLEGIA AND VENTS
Cardioplegia comes in many forms, but it’s basically a high potassium solution intended to achieve diastolic arrest of the heart. Why do we need to arrest? Once the aortic cross-clamp is placed, the heart’s oxygen supply is significantly diminished. Therefore, to prevent ischemic damage, we need also to drive down the myocardium’s metabolic needs for oxygen. This is why we arrest in addition to topically cooling the heart and emptying it (less ventricular distention = less wall stress = less oxygen demand).
Cannulas are placed in the aortic root (antegrade) and the coronary sinus (retrograde). Antegrade cardioplegia perfuses coronary arteries the same way that blood normally perfuses them. The solution is infused into the aortic root, where the left main and right coronary arteries come off just above the aortic valve’s leaflets. It relies on a competent aortic valve. Otherwise, cardioplegia solution would drop back into the left ventricle (LV), increasing wall tension, myocardial demand for oxygen, and ischemic damage. This is why vents are placed. An LV vent is typically advanced from the right superior pulmonary vein (RSPV) into the left atrium, through the mitral valve, and into the LV to keep it empty. The antegrade cardioplegia cannula also doubles as a vent for the aortic root too. Vented blood rejoins the venous reservoir at the beginning of the CPB circuit.
Retrograde cardioplegia is infused through a cannula in the coronary sinus – the common venous drainage for most of the coronary network. This cannula is placed within a small venous structure, so we transduce a pressure off it to a.) ensure proper placement and b.) keep the infusion pressures low to avoid coronary sinus damage.
Surgeons will work with the perfusionists to achieve a good diastolic arrest with antegrade and retrograde cardioplegia before going further. As you can see, mitigating the oxygen supply/demand mismatch is accomplished by cooling, venting, and arresting the heart.
As always, drop me a comment below with any questions or suggestions! 🙂






Why do we cannulate the Aorta first? Can you provide a more thorough explanation in regards to “in case we have to crash onto bypass?”
I find this answer unsatisfying because of how quickly the reservoir will run out without venous return from the patient. Thanks for the help.
Extra volume can be added directly to the reservoir which happens regularly during a bypass run in the form of Cell Saver, crystalloid chase, etc so it doesn’t run dry. This is an option during the peri-bypass period too if the patient becomes unstable and the aortic cannula is already in place.
Hi Rishi! Hello from your big fan in Iowa! I wanted to ask you a question which Ive tried looking for the answer in textbooks but haven’t been able to find one. It is a rather dumb question and I know the answer lies in basic anatomy knowledge. Why do we crossclamp during retrograde cardioplegia? Thanks
Hey Dr. Rishi! Third year medical student here– thank you so much for this post. I’ve had the opportunity to scrub into multiple open heart procedures during my cardio/surgery rotations, and all the tubing, cannulations, and CPB-specific terminology gets confusing in the moment. This was incredibly helpful and succinct.
Hey Julie! Thanks so much for the thoughtful comment! Cardiothoracic surgery is uniquely differently compared to other disciplines due to the additional step of CPB and cardioplegia cannulation before beginning the actual operation. I’m glad you found this post helpful! Best wishes to you! 🙂
Great read. Some was over my head but it was interesting nonetheless. My dad had double bypass in feb 2016.
Thanks for the comment, Donna! Hope your dad is doing well! 🙂