Cardiopulmonary physiology has always been an interest of mine. I’ve previously written about how cardiac output is affected by spontaneous versus positive pressure ventilation, and now I want to discuss how pulmonary vascular resistance (PVR) is affected by ventilation.
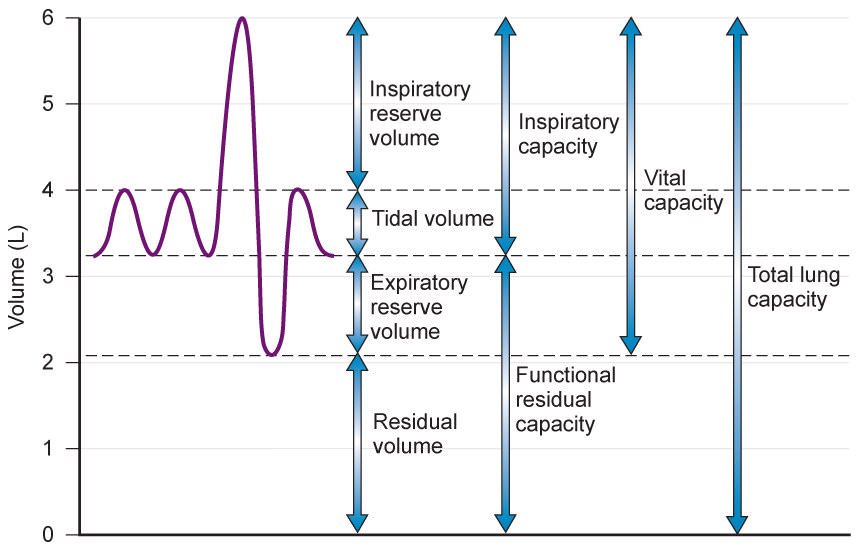
The figure above illustrates the lung volumes and capacities we learn in pulmonary physiology. The first two purple waves represent normal, tidal breathing (what we usually do at rest). A forced inhalation or expiration above or below the tidal volume zone will now incorporate reserve volumes. The key parameter I want to emphasize is the functional residual capacity (FRC) – the air remaining in our lungs after a passive expiration.
At FRC, the inward elastic forces of the lung are in equilibrium with the outward elastic forces of the chest wall. With this definition in mind, pathologies which change these elastic forces will also change the FRC. For example, lung elasticity is significantly reduced in emphysema (a form of chronic obstructive pulmonary disease) thereby increasing FRC and leading to hyperinflation. If these patients are also deconditioned, their chest wall elasticity will also decrease and only worsen the problem.
PVR = [mean PAP – mean PAOP] / CO where PAP is the mean pulmonary artery pressure, PAOP is the mean pulmonary capillary occlusion pressure, and CO is the cardiac output. It represents the resistance blood flow encounters moving from the right to the left side of the heart through the pulmonary vessels. But how does this relate to FRC?
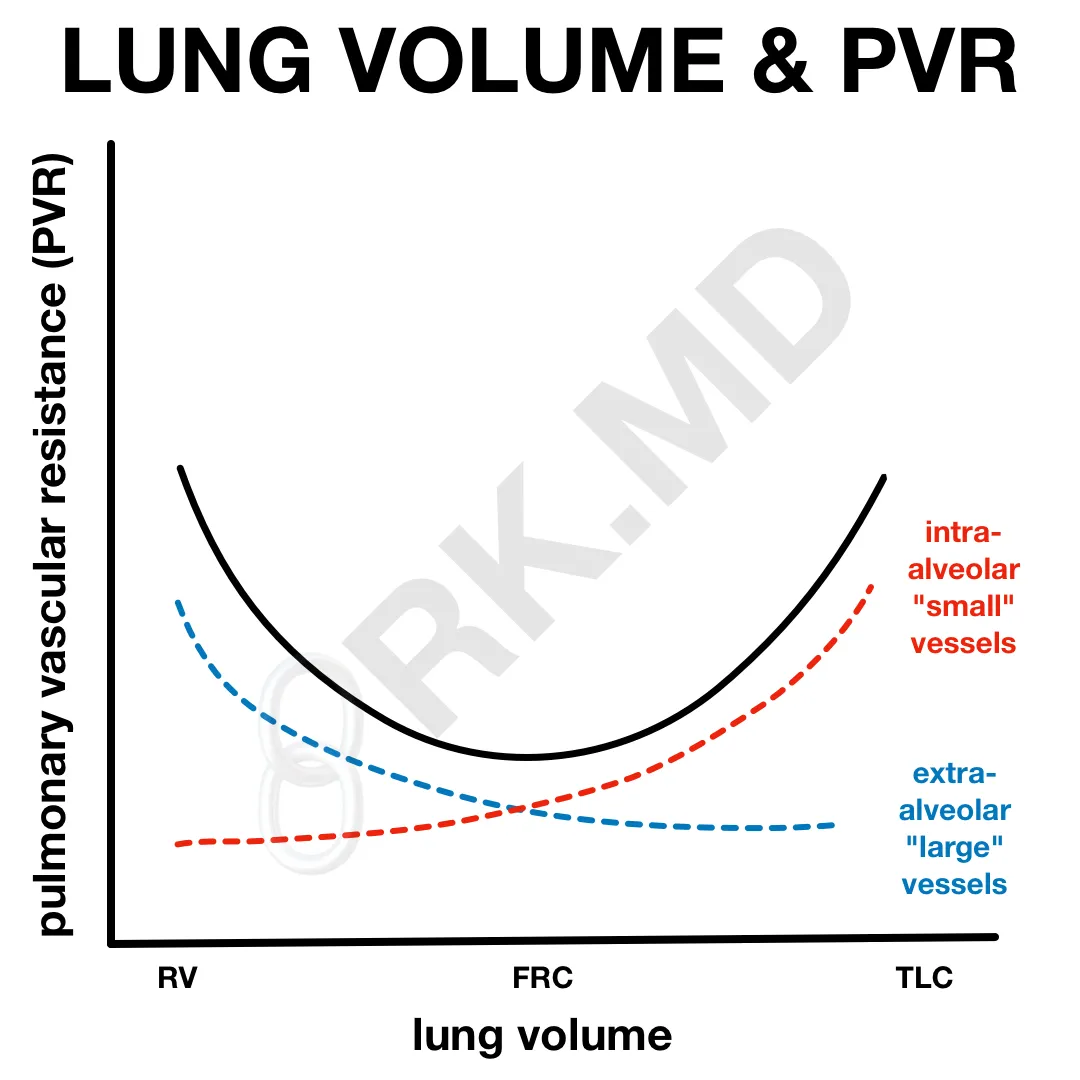
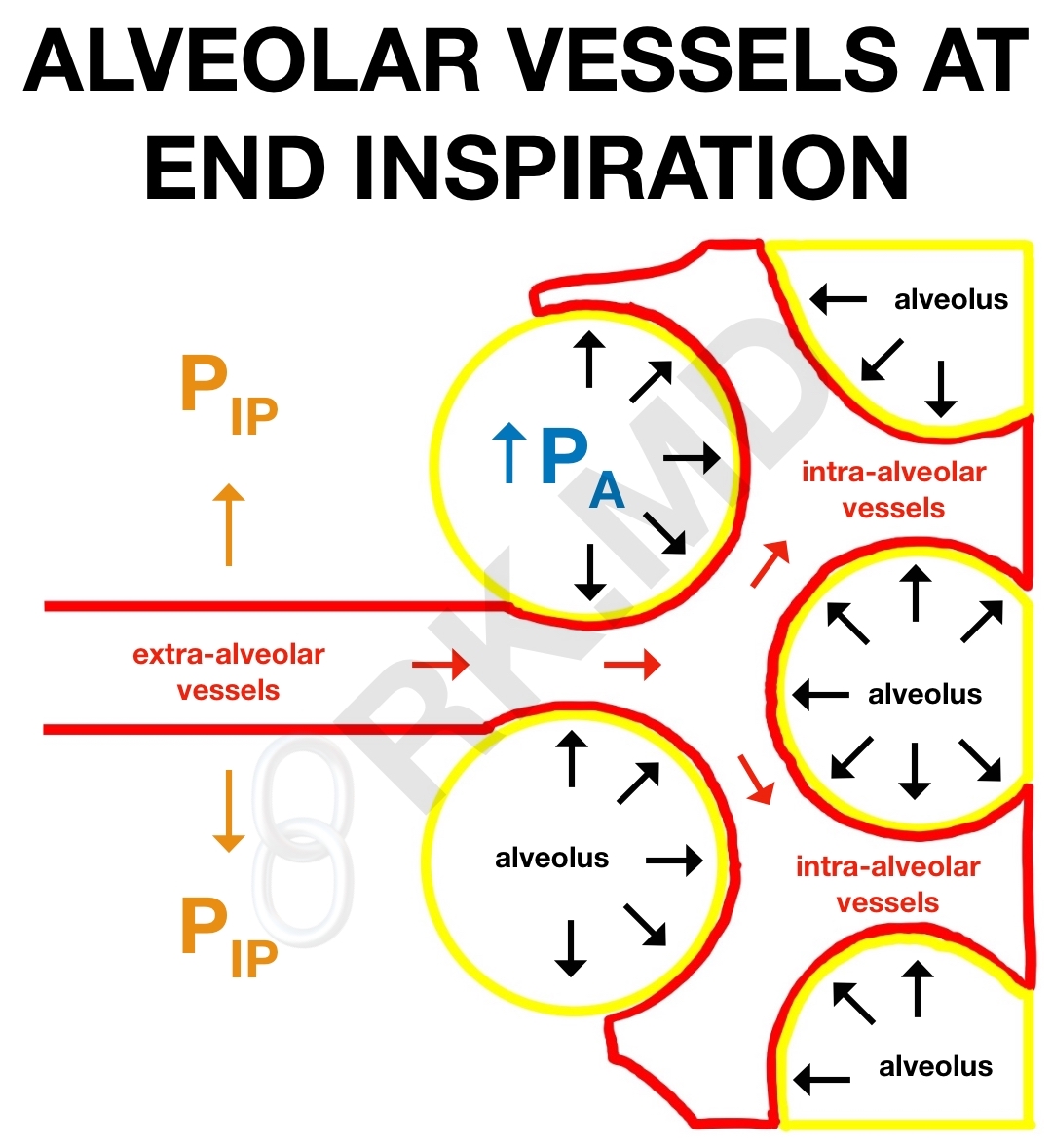
As we fill our alveoli during inspiration and our lung volumes approach the total lung capacity (TLC), blood vessels within the alveoli (intra-alveolar vessels) get compressed leading to increases in resistance. As lung volumes drop, distal airways collapse causing alveolar hypoxia and hypoxic pulmonary vasoconstriction (HPV).
In contrast, blood vessels within the lung parenchyma (extra-alveolar vessels) actually dilate during inspiration due to an increase in radial interstitial forces. In other words, the negative intrapleural pressure (PIP) actually pulls parenchymal vessels open thereby decreasing resistance.
Both intra-alveolar and extra-alveolar vessels serve as channels for pulmonary flow, so their net effect on PVR is represented by the solid curve in the diagram above. At FRC, PVR is at its nadir.
Okay, fine, but why is this important?
Imagine you have a patient with pulmonary hypertension on mechanical ventilation for surgery. Besides the typical treatments (oxygen, avoiding hypercarbia/acidosis, Flolan, nitric oxide, PDE3 inhibitors, endothelin antagonists), it’s imperative that their pulmonary mechanics are monitored closely. Tidal volumes which are either too high or too low relative to the patient’s FRC could worsen PVR and right ventricular afterload potentially precipitating acute right heart failure.






Dr. Kumar,
Is the FRC measurable? Why not have patient’s perform PFTs prior to surgery to better understand their volumes? Or is this overkill? Thanks
Evan
Traditionally, functional residual capacity (FRC) is measured using techniques like body plethysmography, washout/wash-in methods, and helium dilution methods. PFTs aren’t always necessary prior to surgery, but for many operations (ie, thoracic surgeries), they’re often done to help predict perioperative pulmonary complications. In my experience, it doesn’t really change anything in the operative or immediate post-operative setting though.
hello Rishi, I’m a medical student from Italy and i’m working on a project about hemodynamics.
I was wondering why during spontaneous inspiration, the RV afterload drops.
During spontaneous inspiration pleural pressure decreases, so i was expecting transpulmonary pressure and PVR to rise, and so also the RV afterload.
Reading this article i found that’s actually the opposite: during inspiration pleural pressure and transpulmonary pressure decrease, leading to a drop of PVR and RV afterload,
https://www.sciencedirect.com/science/article/pii/S0735109718357279?via%3Dihub#mmc1 .
Could you help me understand this point?
I really look up to you. Thanks!
Hey Giulio! Here’s how I think about it. Transpulmonary pressure (TPP) is the difference in pressure between the alveolar space and the pleural space: TPP = Palv – Ppl. Pleural pressure is always negative (and even more negative during inspiration) whereas alveolar pressure is slightly positive during expiration and slightly negative during inspiration. You can read more about the details (with a diagram) on my other post: How We Breath – The Role Of Pressure Gradients. I also have another post where I discuss how PVR changes over the respiratory cycle here: link to post
Let me know what you think!
Well, nice article regarding a topic i am fond of myself… A couple question though:
How do you adjust tidal volume to FRC when it is intially adjusted to IBW?
How do you closely monitor “Pulmonary mechanics”?
Thanks again
I think less about adjusting things for FRC (it’s positional, dependent on age, dynamic throughout a procedure, etc). The literature supports using low tidal-volume ventilation (6 cc/kg), so that’s what I aim for. My point with this post was to explain how the PVR is affected by varying lung volumes.
I monitor all aspects of mechanical ventilation – peak and plateau pressures, the flow-volume/pressure-volume loops, and the capnogram are the big ones. If there are signs of lung over-distention, breath-stacking, patient dyssychrony with the ventilator, etc, I’ll adjust things accordingly.