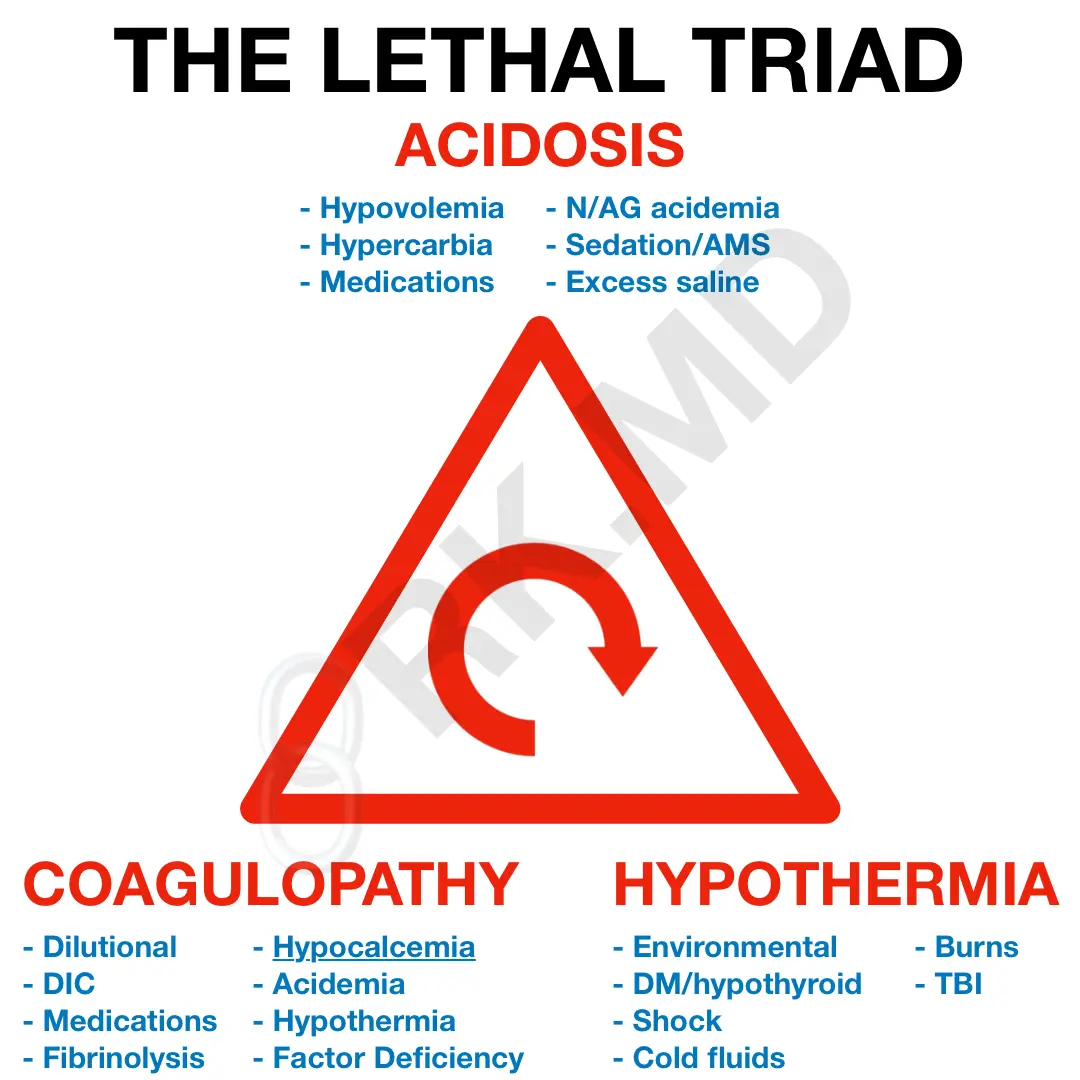
The lethal triad in trauma – acidosis, hypothermia, and coagulopathy – defines much of what I do in the ICU and cardiothoracic ORs. It’s important to appreciate the interplay between these three derangements, anticipate problems, and intervene quickly.
Hypothermia has profound implications on pharmacokinetics, glycemic control, infection risk, wound healing, dysrhythmias, and coagulopathy – a term used to describe a broad derangement in the coagulation cascade. Primary and secondary hemostasis involve numerous, temperature and pH-dependent enzymatic reactions. Therefore, hypothermia and acidosis can impair platelet aggregation and the activation of clotting factors. We’re often so preoccupied with what and how much to transfuse, but we should make temperature management equally important.
In massive hemorrhage, you don’t need an H&H to tell you what your eyes are seeing. We also don’t bleed LR or NS. Fluid of choice should be blood, plasma, and platelets to maintain physiologic proportions. Throw in some calcium too!
Tissue oxygenation can be affected by hemorrhagic/hypovolemic shock and compensatory vasoconstriction in the face of hypovolemia (+/- hypothermia). Resulting anaerobic metabolism can lead to lactic acidosis which can be compounded by massive saline-based resuscitation and a superimposed respiratory acidosis from hypercarbia due to weakness, altered mental status, sedation, etc. Acidosis can cripple the body’s coagulation cascade, cardiac inotropy (fueling the downward spiral of hypoperfusion), and even render many of our resuscitative medications (epi/norepi) and endogenous proteins ineffective.
So what do we do? Stop the bleeding (apply pressure, embolize, stabilize, etc.), preserve normothermia (warm the environment/fluids, use blankets and active warmers), avoid hypoxemia and hypercarbia (secure the airway if needed), consider antifibrinolytics like TXA, and constantly reassess!
Drop me a comment below with questions! Let me know how you deal with the lethal triad in your practice!






Hello Doc… This is Lt. Alden from the Akron Fire Dept. in Akron Ohio. I will be presenting on the Triad at a few conferences soon. How does calcium play a key role in the Triad? Would it be beneficial to implement pushing CaCl for major trauma patients? Please advise and thank you in advance. Sincerely – Lt. Jarred R. Alden, M.A., FFII, NRP
Hi there! First of all, thank you so much for your service. You and your colleagues do incredible work and have my undying respect!
Citrate is added to blood products to help prevent coagulation when stored. During transfusion, this citrate load can lead to systemic HYPO-calcemia. Calcium is an incredibly important factor in the coagulation cascade, cardiac contractility, vascular resistance, etc. Therefore, you’ve gotta keep up with calcium repletion in the background of ongoing blood transfusions!