The word “dialysis” evokes many clinical indications and contexts. In chronic end-stage renal disease (ESRD), patients typically have some form of long-term access like an AV fistula for their scheduled sessions. In the short term, we’re taught indications for dialysis based on the vowels:
- A: intractable acidosis
- E: electrolyte derangements (potassium, sodium, and calcium, in particular)
- I: intoxication (ethylene glycol, methanol, lithium, aspirin)
- O: volume overload
- U: uremic symptoms
Notice that we do not dialyze for elevated creatinine alone.
To be more specific, we need to break renal replacement therapies (RRT) down into hemodialysis and hemofiltration. The former is more often utilized on an intermittent schedule like three-hour sessions on Mondays, Wednesdays, and Fridays. In comparison, hemofiltration occurs more often with much longer RRT sessions like continuous venovenous hemofiltration (CVVH). We tend to use the latter in the ICU setting quite a bit. Let’s discuss each one. 🙂
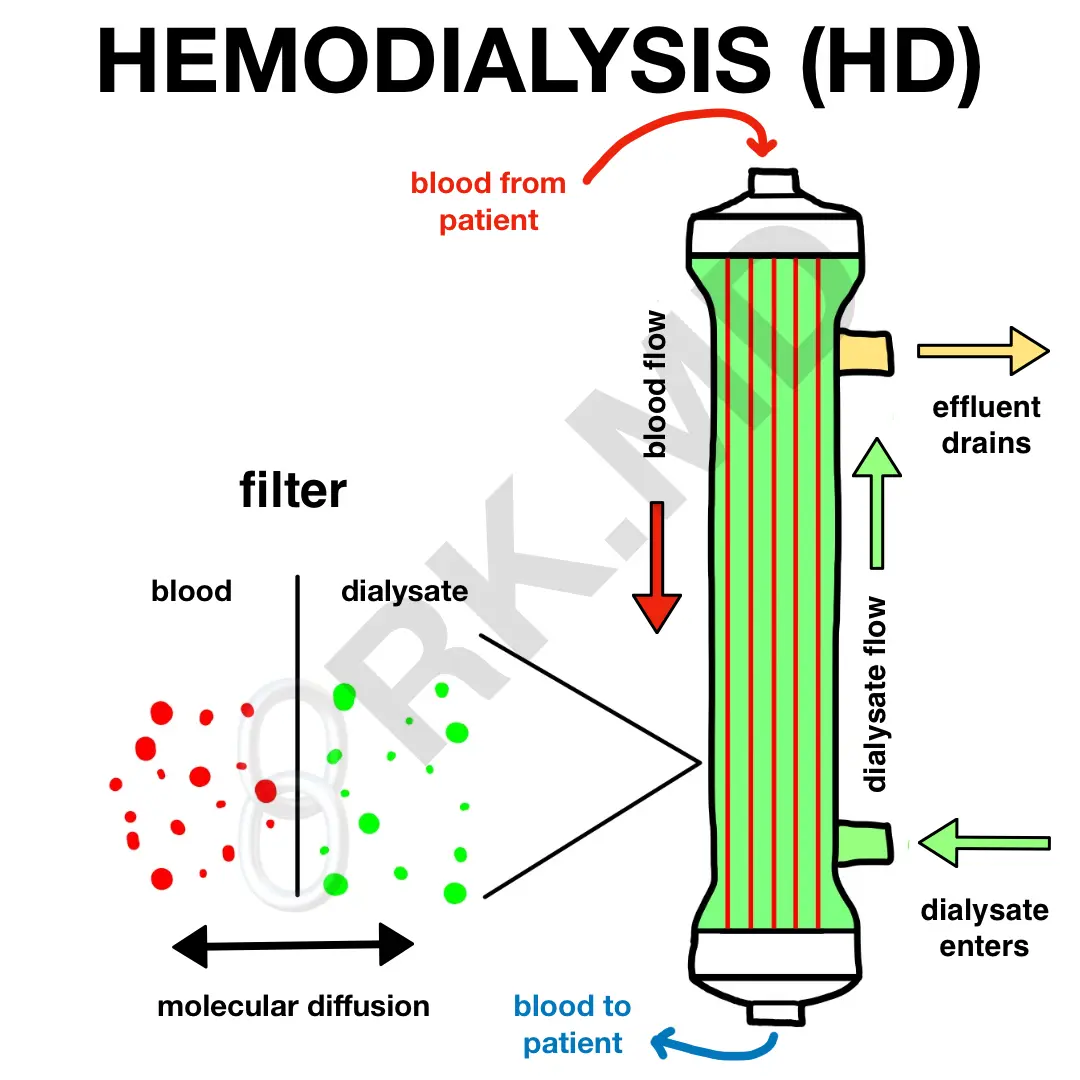
HEMODIALYSIS (HD)
An HD filter consists of many hollow fibers through which blood flows. A dialysate solution consisting of ions of varying concentrations (depending on your goal with HD) flows in the opposite direction and bathes these fibers. Diffusion of small solutes occurs along their concentration gradients through pores along these fibers. The “wasted” dialysate is termed effluent and discarded. To keep things in perspective, a three-hour HD session can use roughly 75 liters of water! 😯
Diffusion across the filter’s pores is dependent on:
- blood and dialysate flow
- concentration gradients
- size (solutes < 5,000 Daltons like urea, sodium, potassium)
- charge
- solute removal is independent of water movement due to diffusion
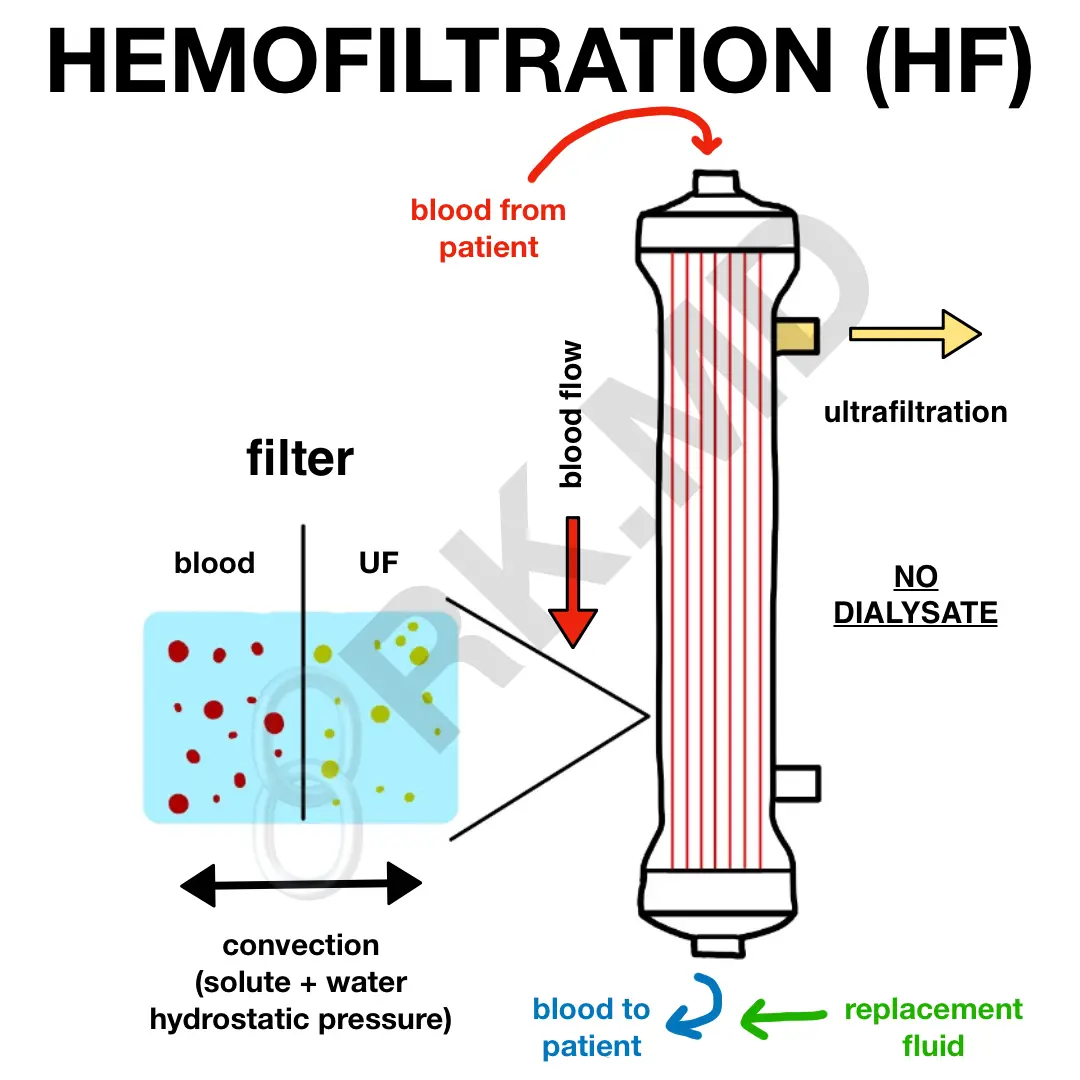
HEMOFILTRATION (HF)
In comparison to diffusion-based HD, HF relies on convection through a larger pore hemofilter. The key difference is the absence of dialysate. Instead, pressure is applied across this hemofilter, and solutes are pushed through the membrane along with plasma water. This removed volume is termed ultrafiltrate and parallels the physiology involving Bowman’s capsule and the glomerular capillary bed. Because of this volume removal, replacement fluid is added back before and/or after the hemofilter (termed pre and/or post-dilution, respectively) to maintain adequate volume status in the patient.
Overall, HF is better at removing solutes from 5,000 – 50,000 Daltons like salicylates, β2-microglobulin, and some inflammatory mediators implicated in sepsis. However, because of convection, solute removal is dependent on fluid removal.
Now let’s take the examples of intermittent hemodialysis (iHD) and CVVH. What are the pros and cons?
iHD is less expensive and permits rapid solute removal but oftentimes creates hemodynamic lability, cerebral edema, and disequilibrium. In comparison, CVVH (a form of UF) is more physiologic, allows the continuous removal of toxins, tends to be user friendly, provides gentle ultrafiltration, and may have a role in immunomodulation by removing inflammatory markers; however, it often requires patient immobilization, prolonged anticoagulation, and is associated with increased costs.
Hopefully you found this useful as a quick primer to renal replacement therapy! Drop me questions below! 🙂






Neatly explained with illustrations .Tq
Glad you like it! 🙂
Thank you SO much for taking the time to explain this.
My pleasure! Glad you found it helpful!
Very helpful posts! Really appreciate you taking the time to teach this
You’re very welcome! Thank you for the comment!