Glycemic control in the perioperative and ICU settings is a crucial consideration for me! As a cardiac anesthesiologist, I routinely start my patients on insulin infusions with a small bolus depending on the severity of their hyperglycemia. Unlike conscious patients that may become tremulous, diaphoretic, or even pass out, patients under general anesthesia don’t show the typical “signs” of hypoglycemia. Instead, their first symptom might be hemodynamic collapse – a differential that involves plenty of causes (especially in the cardiac ORs) well before hypoglycemia. Therefore, it’s important to check how a patient’s glucose is trending!
As an intensivist, I often find myself transitioning patients with diabetes on high-dose insulin drips to an alternative regimen. Basal-bolus insulin (BBI) and insulin sliding scales (ISS) tend to be proactive and reactive approaches to glycemic control, respectively, but using a combination tends to smooth things out. I estimate my patients’ total regular insulin requirements in a day (i.e., 150 units), take 70% of that (105 units) and divide that 50:50 into long-acting insulin (detemir or glargine) and regular insulin every 6 hours if they are receiving continuous tube, feeds and/or have fluctuating oral intake. If they have a stable, three-meal diet, I substitute rapid-acting insulin (lispro or aspart) before each meal.
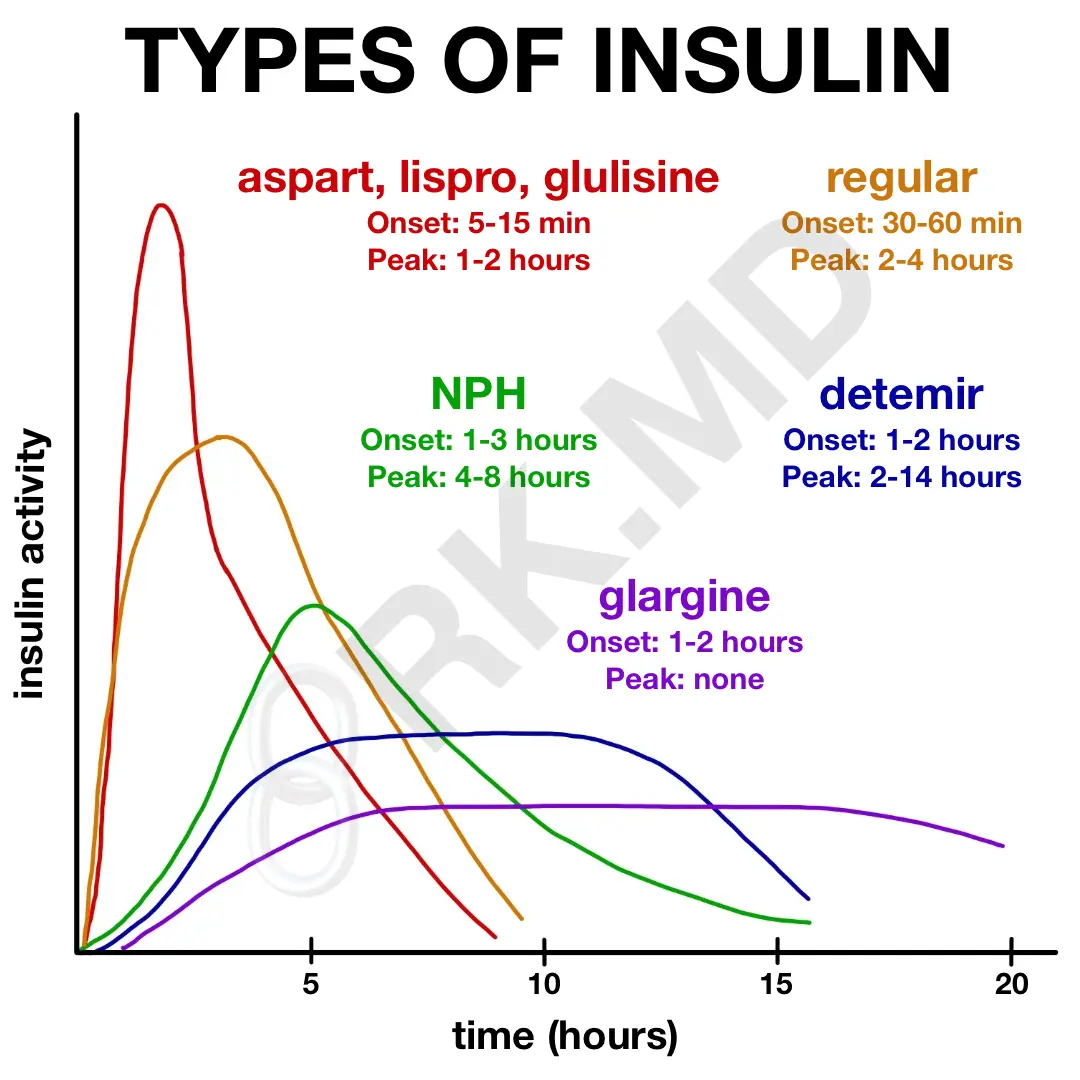
Inpatient glycemic control can be incredibly challenging, so it’s important to understand the peak onset/duration of different kinds of insulin (in the diagram), seek advice from specialists, and provide good education to your patients!
Drop me a comment below with questions! 🙂