Deep hypothermic circulatory arrest (“circ arrest”) is often required for partial or total aortic arch reconstructions. At this point in the surgery, there is no blood flow anywhere. Because of systemic cooling, we mitigate the anaerobic and calcium-mediated apoptotic pathways that are implicated in neuronal dysfunction and can safely perform surgery for short circ arrest periods.
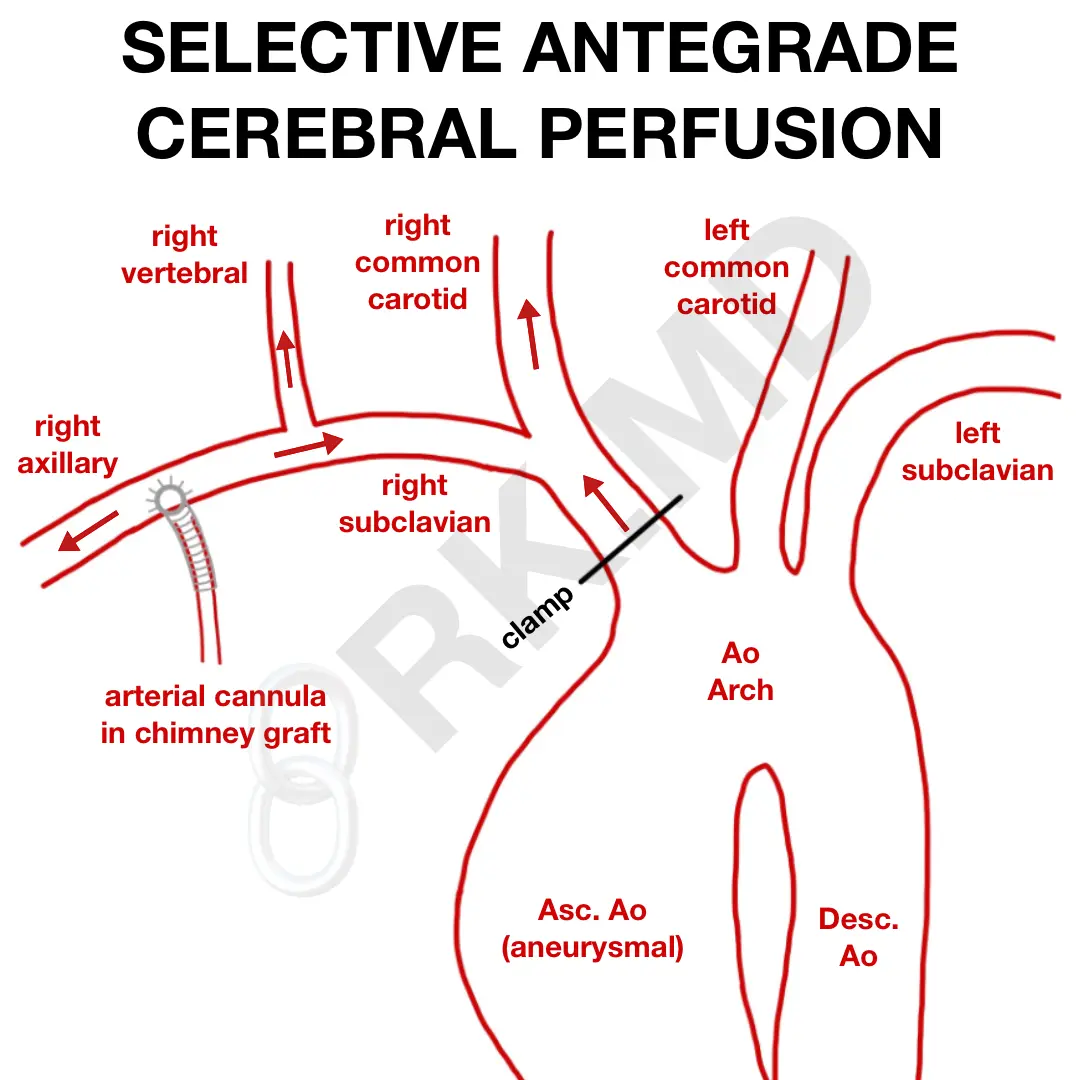
If a longer circ arrest period is expected, selective antegrade cerebral perfusion (SACP) is a technique that maintains brain perfusion and relies on collateralization through the Circle of Willis to perfuse the contralateral left brain. In one approach, a chimney graft (ie, 8 mm Dacron) is sewn to the right axillary artery and perfused with an arterial cannula that connects to the cardiopulmonary bypass (CPB) circuit. Initially, this cannula perfuses the entire body through the graft with ~50 cc/kg/min of flow.
After the heart is arrested with cardioplegia and moderate systemic hypothermia is obtained, a clamp is placed proximally on the innominate artery and flow is lowered to ~ 10 cc/kg/min. Now the arterial cannula is only able to perfuse down the right arm and up the right vertebral/carotid systems into the brain. For this reason, a right radial arterial line pressure serves as a surrogate for cerebral perfusion pressure.
Drop me a comment with questions below! 🙂






what are the advantages and disadvantages of Antegrade & Retrograde Cerebral Perfusion
Would you require to vent the heart with both antegrade and retrograde cerebral perfusion? if so where and why?
Yeah, most commonly the left ventricular vent is placed through the right superior pulmonary vein (RSPV → left atrium → mitral valve → left ventricle). The vent keeps the left ventricle decompressed which is important to reduce wall stress caused by chamber distention and, in turn, reduces myocardial oxygen demand.
How would the rest of the body, more specifically the left side be perfused if we’re only focusing on cerebral perfusion? Would we rely on DHCA for everything else?
You’re relying on an intact Circle of Willis for flow to get to the left cerebral hemisphere from the right-sided circulation. DHCA should cover everything else.
What role do you think cerebral ox plays in DHCA? it is reliable?
Thanks!!
It’s just another tool. High cerebral sats could be indicative of adequate oxygen delivery and/or poor oxygen uptake (ie, decreased metabolism, as seen with DHCA), so how “reliable” something is depends on what you’re actually trying to assess. Some places will use BIS monitors to ensure EEG silence prior to beginning DHCA too (although that has its own issues… namely that you’re really only looking at a modified frontal EEG).
Whats your opinion on some Surgeons choice to only cool to 28C or 24C for DHCA? Do you think theres a big difference between 18C and 24C?
Also how did they come up with these flows? Why 10cc/kg/min?
I’m not sure exactly where the 10 cc/kg/min came from, but it makes sense that it’ll be lower than the traditional 50 cc/kg/min which is often used for full, systemic perfusion since with ACP, only the right arm and brain are being perfused. As far as temperature, I know that 18-20C is generally regarded as safe, but cooling to that degree comes riddled with the usual issues of DHCA (not to mention a longer re-warming). Here’s a paper that suggests moderate hypothermia (24C) + ACP may provide superior neuroprotection to DHCA at 18C alone.
Thanks for sharing it, was really helpful for me!!!