Although small amounts of air and fluid in the pleural space are generally well tolerated, pneumothorax, hemothorax, chylothorax, etc., necessitate chest tube placement. Smaller bore tubes can often be utilized and placed more apically for large air collections as air rises. Viscous fluid collections (complicated effusions, hemothorax, empyema, etc.) often require large bore tubes in the dependent lung base(s) since gravity pulls the fluid to these regions.
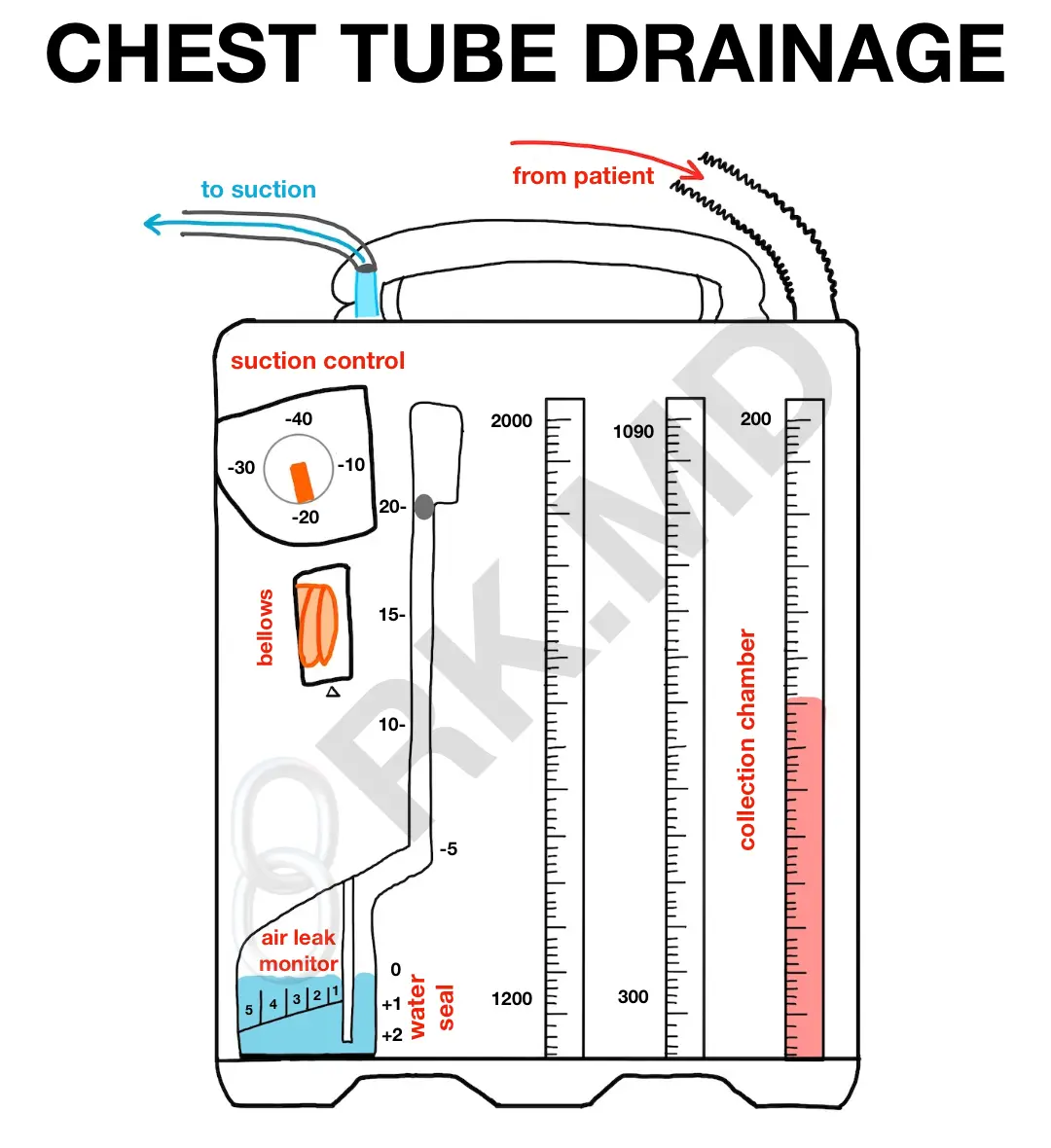
After placing a chest tube, it’s connected to a drainage system like an Atrium (which I’ll reference in this post). This closed system consists of a collection chamber, a water-seal chamber, and a suction control.
COLLECTION CHAMBER
This chamber collects and measures output which can be marked at regular time intervals. The characteristics of the output can also be visually assessed (ie, milky chylothorax after initiation of nutrition may suggest thoracic duct injury). Remember that a drop of blood in a bucket of water will tint the entire thing red, so not all “red drainage” is considered “sanguineous.” Always ensure an airtight seal between tubing interfaces with adapters, tape, and zip ties.
WATER-SEAL CHAMBER
Remember that during a normal, spontaneous inspiratory breath, the diaphragm contracts downward, increasing intrathoracic volume while simultaneously creating a “negative pressure” relative to the outside world. Airflow is directed into the lungs from the environment down a pressure gradient. What’s to say that air can’t be pulled back into the chest via a tube sitting in the pleural space? The water-seal!
The water-seal chamber serves as a one-way valve – air can escape from the pleural space but cannot reenter. This is accomplished by maintaining a column of sterile water at 2 cm in the Oasis systems. Remember that normal tidaling (water level rises with inspiration and falls with expiration if spontaneously ventilating, opposite if receiving positive pressure ventilation) means that this chamber can “see” the pleural space pressure changes suggesting the chest tube is patent. Vigorous, constant bubbling in this chamber suggests a persistent air leak (bronchopleural fistula, pneumothorax, etc.)
SUCTION CONTROL
Suction is applied via the suction port, and suction strength can be directly toggled on drainage systems like the Atrium (typically -20 cm H2O ). Bellows will also expand, confirming the integrity of the suction system.
When we “water seal” a patient, suction is removed and drainage is monitored to gravity along with signs of air reaccumulation (repeat chest x-ray in a few hours, symptoms of dyspnea, etc.) Depending on the physician’s preference and clinical circumstances, this is often a good test before removing the chest tube.
I look for things as an intensivist when examining patients with chest tubes connected to Atrium drainage systems.
- How does the site look? Is it oozing? Does another stitch need to be placed? Does the dressing need to be changed or reinforced? Are the tube’s outermost drainage holes still within the pleural space on the chest x-ray? Is there a chance that the drain is not well situated WITHIN the fluid collection?
- Let’s follow the tube to the drain: are there any clamps, large clots, tube kinks, etc., that will limit drainage? Although I’ve seen countless colleagues “milk” chest tubes to remove debris, there hasn’t been any evidence supporting this practice. One can create negative pressure within the tube transmitted back to the pleural space.
- Is the Atrium BELOW the site of drainage? Remember, gravity is your friend! Is it stabilized against something like a bed frame or IV pole?
- Is the water seal chamber appropriately filled to 2 cm? Remember, less water = less suction pressure. Do I see tidaling or a persistent air leak?
- Is the suction tubing connected (or not connected) appropriately? I ensure the suction port is broken off or taped over in post-pneumonectomy patients for safety. Inadvertently applying suction can result in significant mediastinal shift with possible cardiopulmonary consequences.
- Are there clamps available nearby?
Now let’s talk about accidents/emergencies surrounding chest tubes:
- If the tube is disconnected from the drainage system, immediately clamp it! Depending on hospital policy, the entire chest tube may need to be replaced or the ends of the tube and drainage system sterilized before reconnection. I’m paranoid about properly securing tubes to the drainage systems with zip ties!
- If the tube falls out entirely from the chest, immediately apply an occlusive dressing like Xeroform gauze at the end of expiration. If this is done after inspiration, air entrained in the pleural space through the chest wall defect may become trapped (pneumothorax).
- An acute increase in bright red blood suggests an active bleed. In the immediate postoperative period, this can sometimes be managed by fixing coagulopathy but often requires re-exploration of the chest.
As far as clamping the chest tube, if I see an air leak that doesn’t make sense, sometimes I’ll briefly clamp the tube at the exit point of the chest. If the leak persists, the leak is somewhere in the system itself. Chest tubes are also briefly clamped as the drainage system is changed.
Hopefully, this post addresses some basic points surrounding chest tube drainage systems! Drop me a comment with questions! 🙂






My mother just had her drain tube disconnect and fall on hospital floor. They cleaned the tubing and reconnected it. It wasn’t the actual chest tube but the connecting drainage tube. Is this proper care. Why wouldn’t they just replace the drain hose? Seems very unsanitary to just clean ends of tube and reconnect.
Hello! Great information, thank you for sharing. Question about connecting to wall suction.. What are your thoughts on connecting to the plastic wall suction canisters rather than hooking them straight to the wall unit vacuum regulator? I have heard mixed stories. I had one trauma doctor who despised hooking through the wall suction canister instead of a vacuum regulator.
Really haven’t given much thought to it beyond making sure the suction control is appropriate and the bellow expands.
Hi Rishi,
Question about a patient having a chest tube on wall suction. If they are independent and want to go to the bathroom, would it be appropriate to remove the wall suction for a few minutes, so they don’t have to carry the chest tube with them? Would you need to clamp the chest tube in that case for that brief amount of time?
Hey Sarah, I’m not sure if I’m understanding the question correctly – if you disconnect the wall suction, the chest tube and the drainage system would still be connected to the patient. I wouldn’t clamp and disconnect the chest tube from the drainage system unless I’m planning on exchanging the Atrium. If you’re asking about just taking a patient off wall suction for a few minutes, it really depends on the indication for the chest tube and the severity of the pathology. For example, if a patient has a chest tube because of a recent tension pneumothorax and has a persistent air leak in their drainage system, I’d be more reluctant to remove the suction due to reaccumulation of the pneumothorax. If it’s a patient with a chest tube for post-op fluid drainage, and the drainage has been minimal, I’d be less worried. Not medical advice – just my two cents. 🙂
Hi, I’d like to ask one or two questions regarding the mechanism of the three-chamber chest drainage system.
1) It is usually said that the level of suction is controlled by the depth of insertion of the air vent tube into the water. What is the mechanism by which the height of the column of water controls the amount of suction? I mean, how exactly does the height of the column of water control the level of suction? I have been trying to understand it but it’s difficult for me to figure it out.
Normally, suction force is created when there is a negative pressure. How does a column of water generate the negative pressure required to produce suction?
2) Why do we allow atmospheric air through the vent into the suction chamber? What’s the purpose of the atmospheric vent in the suction chamber of a wet suction?
I’d very much appreciate it if you could clarify these question me.
Thanks.
Are you using zip ties like plumber’s hose clamps?
As usual, thanks for the informative post!
More like zip ties from a hardware store for tying cables. As far as I know, plumber hose clamps (which I’ve used around the household over the years) have a screw locking mechanism.
This is just amazing post
i have question regarding blocked chest tube , like clot , and not draining anymore
how u troubleshoot a clot or blockade in a chest tube ?
I don’t think there are any published “standards” for how to do this, and it seems that although the literature has shown milking/stripping chest tubes to mobilize clots and other debris within the tube lumen can cause tremendous back pressure within the pleural space, it’s still a common practice. If I’m that worried about a clot causing drainage, I suppose one can briefly clamp the tube upstream (close to the patient), try to milk the clot out, and then unclamp the tube. I’d love to hear what other people do!
I’ve also been taught to milk the tube but your suggestion makes more sense. Have you incorporated this suggestion into practice? Also, would you try to apply a STERILE occlusive dressing to the chest tube site if it falls out with sterile gloves or is timing more of the essence?
Yes I have. If the chest tube is still necessary, I’ll replace it. If not, then yes, I’ll place a sterile, occlusive dressing (Xeroform with a Tegaderm usually works well).