Lumbar drains are a mainstay for spinal cord protection when patients undergo operations like thoracoabdominal aortic aneurysm (TAAA) repairs and thoracic endovascular aortic repairs (TEVAR) with subclavian artery debranching. Why? Because the anterior spinal artery receives contributions from paired intercostal arteries that can be disrupted by the aortic pathology itself in addition to the operation (ie, not all the intercostals are re-anastomosed to grafts). So now we have an anterior spinal artery at risk for ischemia.
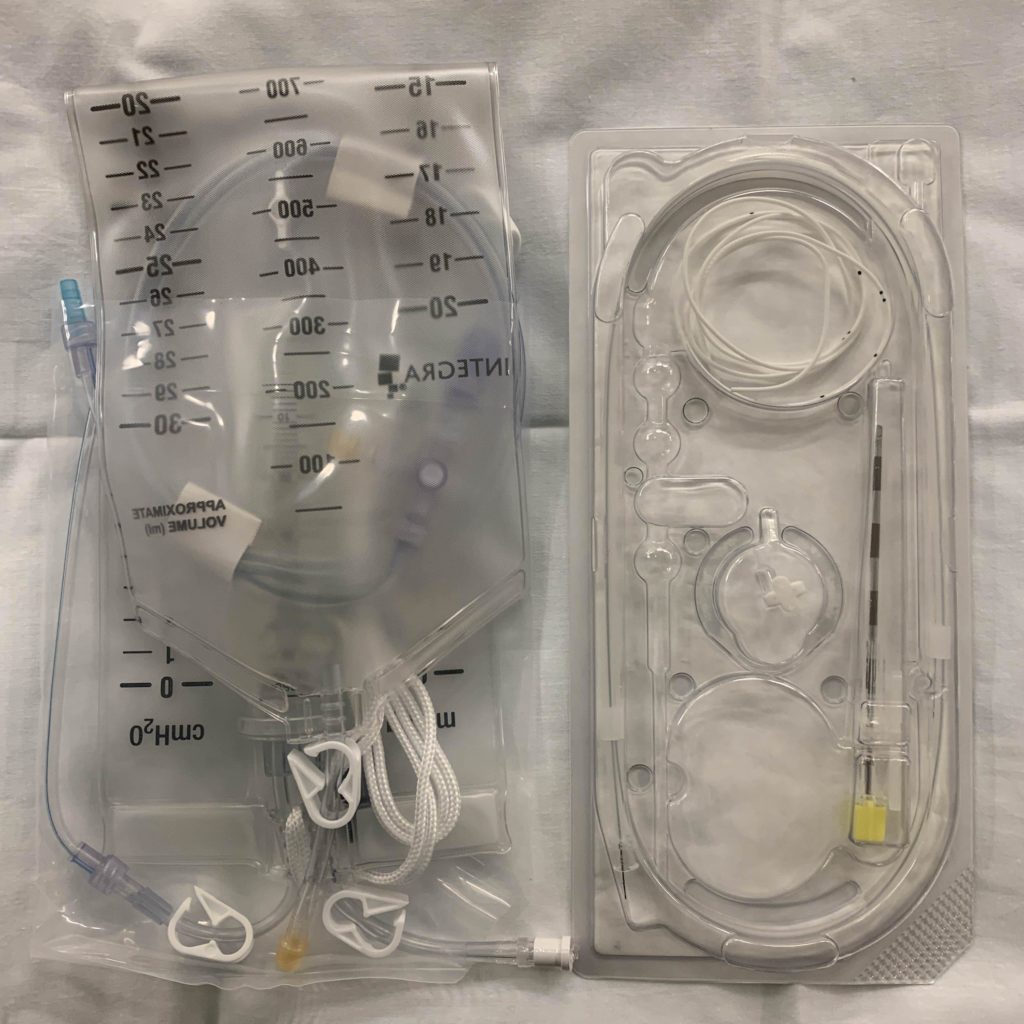
Cardiothoracic anesthesiologists routinely place lumbar drains for these procedures to facilitate the controlled removal of cerebrospinal fluid (CSF). These drains are placed similar to epidural catheters which are often used to control labor or post-operative pain. However, a key difference is a larger Tuohy needle (14 gauge!) is used to access the subarachnoid space where the CSF lives. After this space is entered, a flexible, multiorifice catheter is threaded into the space and connected to a pressure transducer and collection bag system. I use a silk tie to reinforce the connection between the catheter and pressure tubing. I also use Tegaderm and tape to make sure the catheter skin insertion entry point is visible but protected!
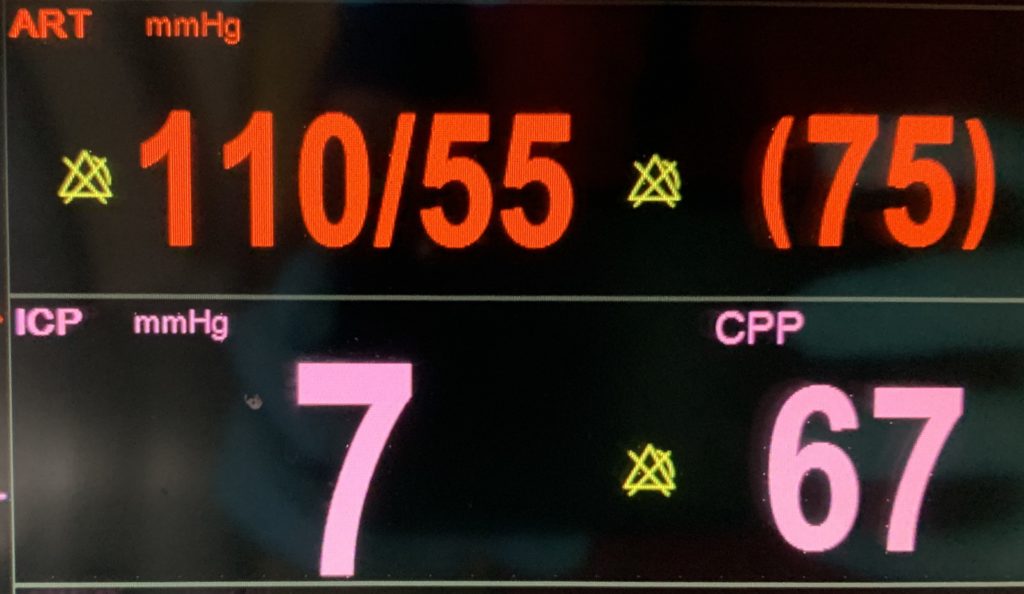
Spinal cord perfusion pressure (SCPP) is determined by the gradient between mean arterial pressure (MAP) and intraspinal pressure (ISP). In other words: SCPP = MAP – ISP. With the lumbar drain in place, I can decrease ISP by intermittently draining CSF (usually no more than 5-10 cc/hr) or using pharmacologic therapy to increase the MAP. These techniques will help improve spinal cord perfusion; however, they’re no substitute for performing lower extremity motor exams post-operatively!
Drop me a comment below with questions! 🙂






So, by controlling the pressure inside the spinal cord, you are able to monitor the surrounding artery status?
The definitive way to really monitor if the spinal cord is experiencing ischemia is by evaluating somatosensory/motor evoked potentials when the patient is under general anesthesia. If they are awake, we can just ask them to move their legs. We can increase mean arterial pressure and decrease intraspinal pressure (by draining cerebrospinal fluid) with the aim of maintaining cord perfusion.
Very concise knowledge, thank you. Skillful tap there Dr. Rishi.
Appreciate the feedback!