Managing elevated intracranial pressure (ICP) is of paramount importance in neurocritical care. Placing bedside ICP monitors are contraindicated if the patient is coagulopathic, has a brain abscess, or has an active scalp infection. Otherwise, the procedure is fairly straightforward and usually boils down to two choices: a Codman ICP monitor (aka, “bolt“) or an external ventricular drain (EVD).
The bolt is a catheter with a strain gauge tip which sits in the brain tissue (parenchyma). Strain gauge basically means a change in force applied to the tip (ie, changes in ICP) will concurrently change electrical resistance within the catheter. FYI, it’s called a “bolt” because a bolt literally affixes the catheter at the cranial suture line.
In comparison, an EVD sits in the third ventricle or lateral ventricles and can be used for measuring ICP as well as therapeutic purposes when draining cerebrospinal fluid (CSF). EVDs are more invasive and often times more difficult to place if the ventricular network is displaced or collapsed.
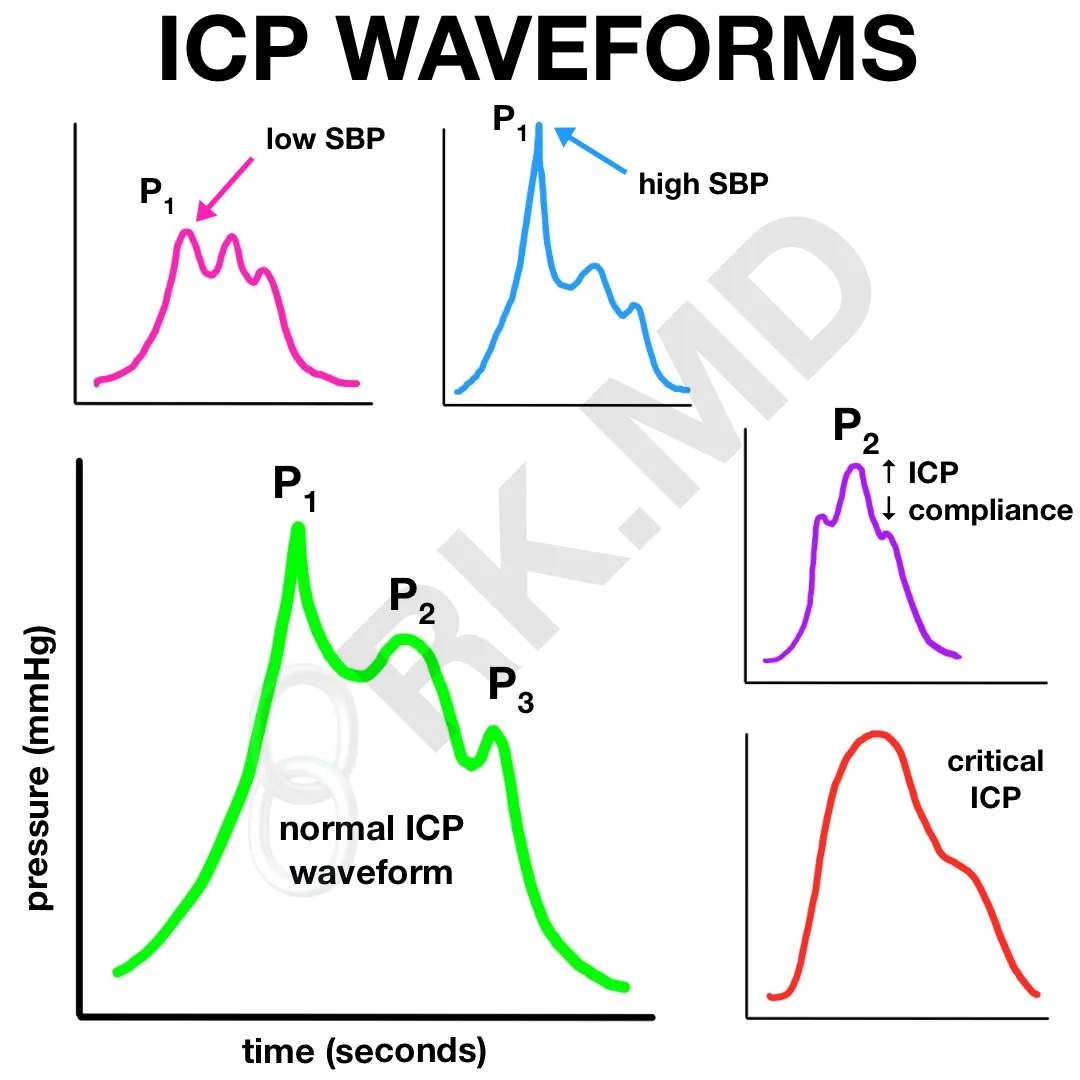
Both the bolt and EVD can transduce a waveform which has some similarities to an arterial line (A-line) waveform. In the normal waveform above, P1 is the “percussion wave” and represents arterial pulsation just like the initial upstroke on an A-line. P2 is the “tidal wave” (cool name, 😎 ) and represents intracranial compliance. Compliance is defined by change in volume / change in pressure, so a poorly compliant brain will accept any additional volume (blood, CSF, brain swelling) by rapidly increasing ICP. P3 is the dicrotic wave, represents a reflected pressure wave due to aortic valve closure, and is analogous to the dicrotic notch on an A-line.
Another important aspect to understand is that the waveform’s overall amplitude will depend on CSF volume. If you’ve just drained a large amount of CSF with an EVD, the new waveform amplitude will decrease in comparison to before drainage. The opposite is also true – accumulation of CSF will augment the waveform amplitude.
Drop me a line with any questions below! 🙂






Rishi As katie stated so elegantly I too would like to use you images to portray ICP waveforms and I was wondering if you have any ICP over ABP over EKG images. I have struggled with finding them to reinforce how the cardiac rhythm affects the ICP
Thankyou for your work and expertise
M
Please use whatever you’d like with the appropriate credit! 🙂 Unfortunately I don’t have any ICP over ABP/EKG images.
Hello! I am a nurse Educator with a background in Neuro Critical Care. I love your article, “MEASURING AND INTERPRETING INTRACRANIAL PRESSURE (ICP) WAVEFORMS.” It is short, sweet, and to the point! Just the way I like to teach my new ICU nurses. I am developing new content and with your permission, would love to use the colored various ICP waveform picture. With the appropriate reference of course! Thanks so much! Keep writing the short and sweet educational tidbits!
Hey Katie! I’d be very humbled if you used my content for the purpose of educating others! You have my permission! 🙂
Hi Rishi,
I came across your website while researching ICP waveforms. I am a cardiovascular perfusion student and I was interested in knowing if you come across ICP monitoring devices in the cardiothoracic OR often? And if so, what kind of patient needs this?
Hey Nathan! For many of our surgeries involving open or endovascular repair of the thoracoabdominal aorta, the cardiothoracic anesthesiologists place lumbar drains to transduce and drain cerebrospinal fluid during the case as well as post-operatively. When I’m in the OR, I’m more interested in the overall CSF pressure, but when I’m rounding in the ICU, I do like to nerd out over the waveforms. 🙂