Here’s a quick primer of cardiac transthoracic echocardiography (TTE) including actual images I’ve taken as a critical care fellow with corresponding labeled diagrams. I challenge you all to actually review your patients’ echo images instead of reading the final impression. You don’t need to know the nitpicky numbers, gradient assessments, valve areas, etc. Knowing what you’re looking at, reviewing enough examples, and THEN looking at the final report will be helpful in knowing how to “eyeball” future scans.
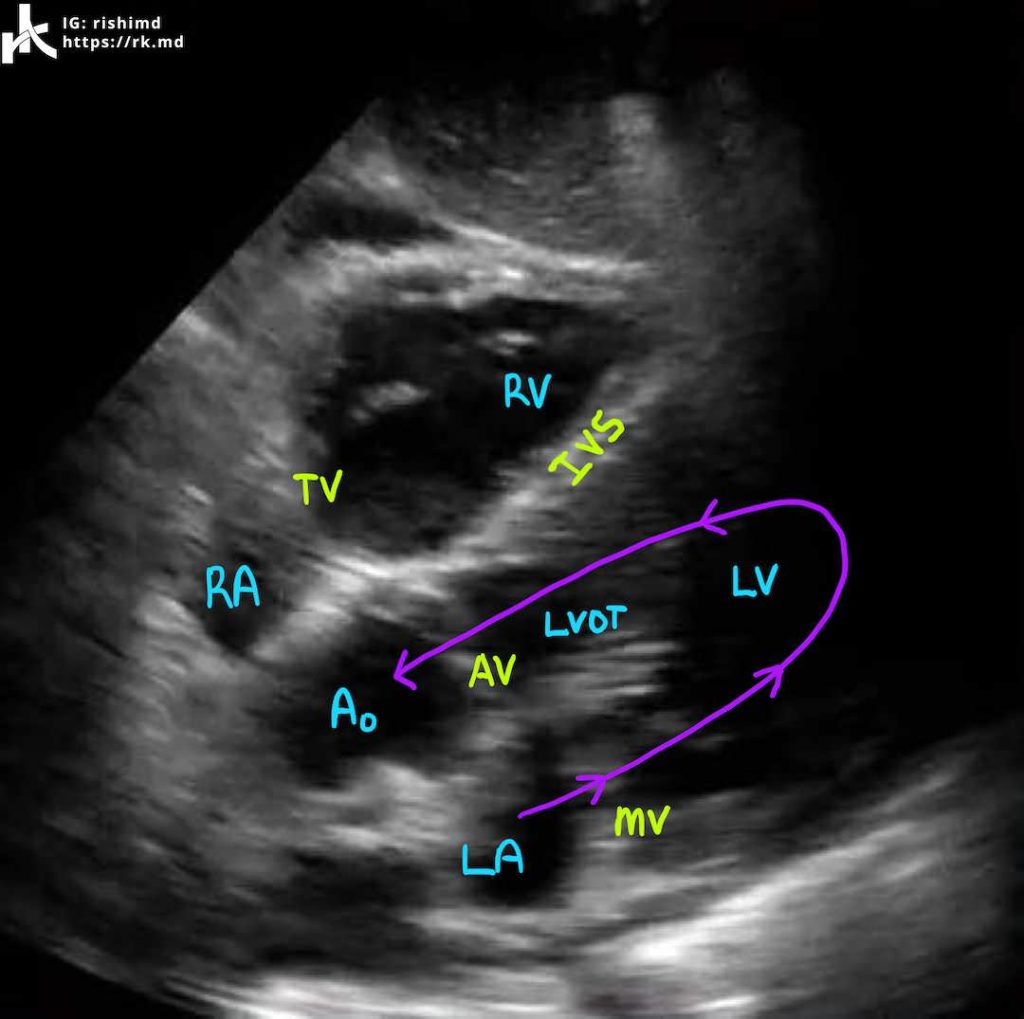
PARASTERNAL LONG AXIS (PLAX)
The parasternal long axis (PLAX) view is ideally obtained with the patient in the left lateral decubitus position with the ultrasound probe placed in either the 3rd, 4th, or 5th intercostal space on the left sternal border (around the sternocostal angle) with the probe indicator pointing to the patient’s right shoulder.
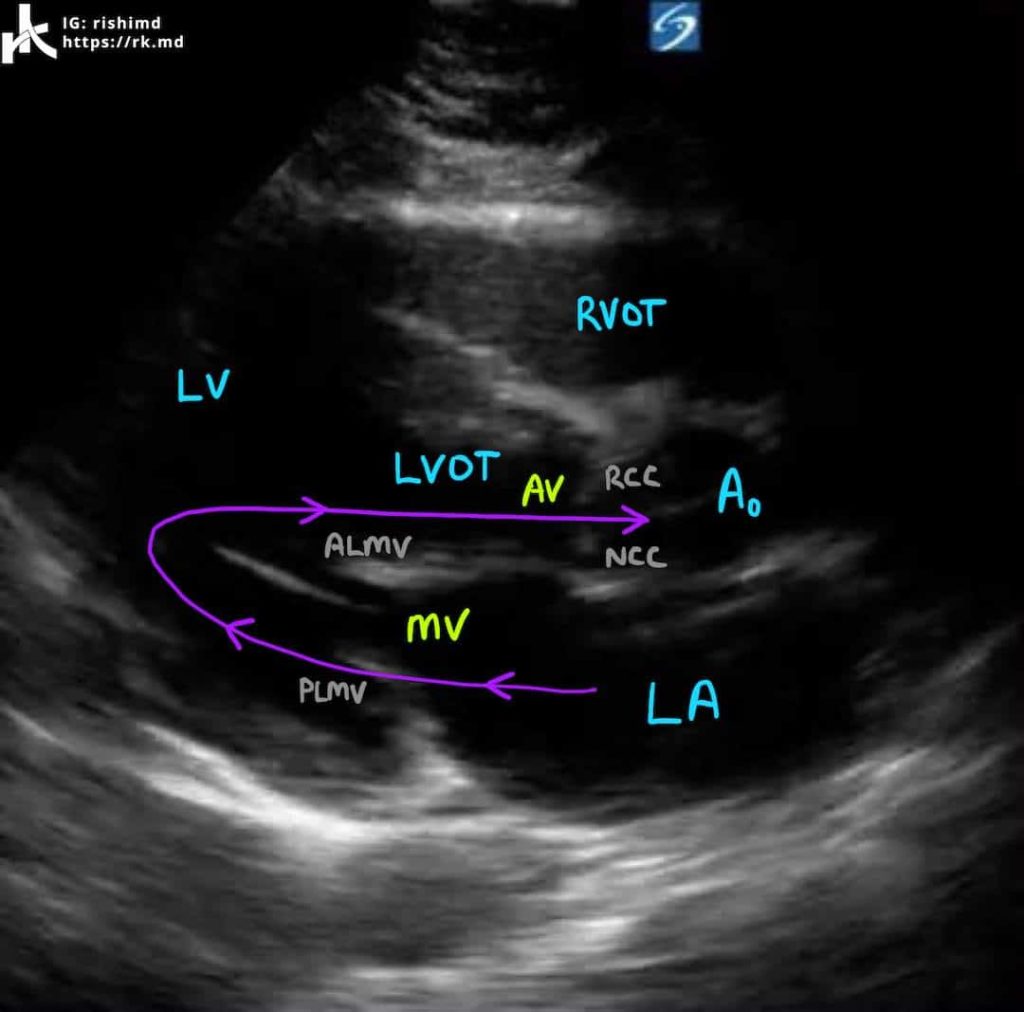
This view is great for quickly evaluating the contractility and chamber size of the left ventricle (LV) and right ventricular outflow tract (RVOT) as well as the function of the aortic valve (AV) and mitral valve (MV). We can also (usually) see the right coronary cusp (RCC) and non-coronary cusp (NCC) of the AV as well as the anterior and posterior leaflets of the mitral valve (ALMV and PLMV, respectively).
Blood flow travels from the left atrium (LA) through the MV into the LV during diastole and from the LV through the left ventricular outflow tract (LVOT) and AV into the ascending aorta (Ao) during systole. Using color doppler to assess gradients across valves is riddled with error as the ultrasound beam is almost perpendicular to blood flow. During diastole, we can measure the LV’s diastolic cavity, aortic root diameter, and diastolic septal and posterior LV wall thicknesses. During systole, we can measure the LA and LV diameters.
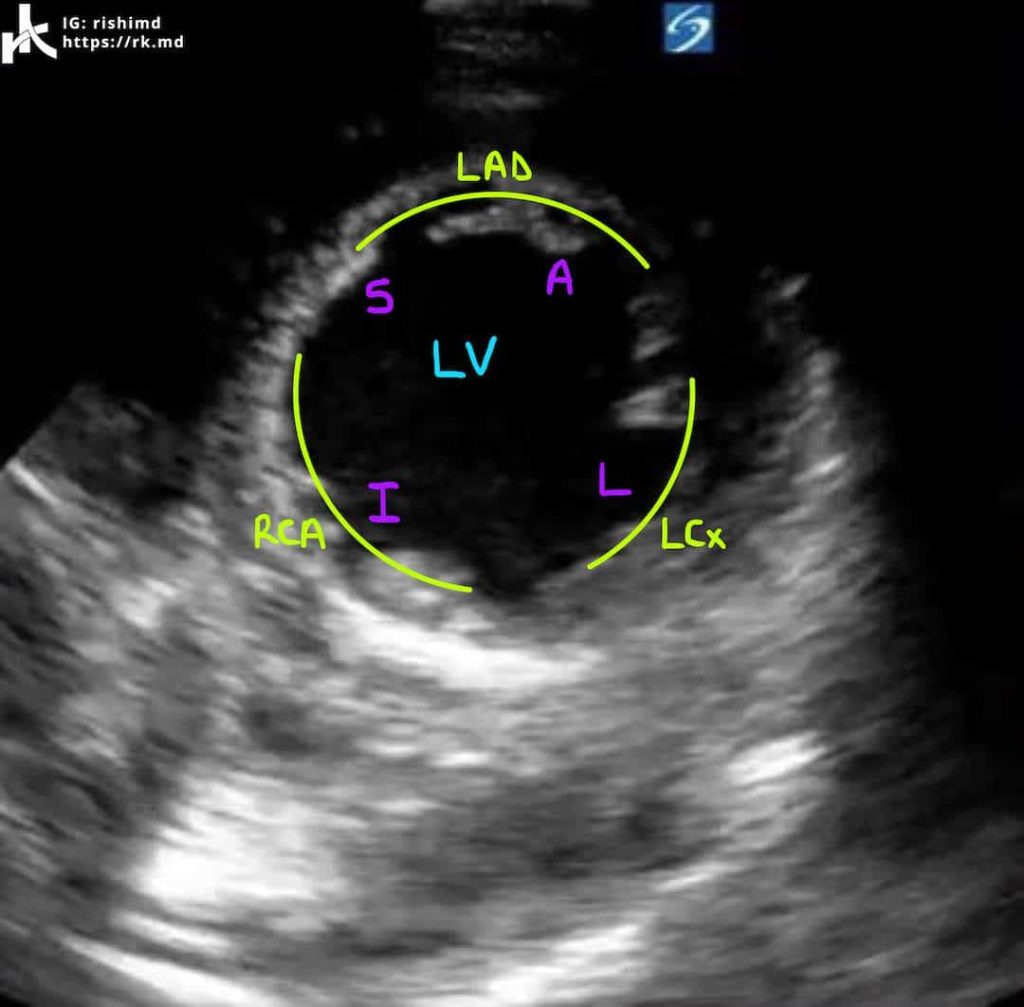
PARASTERNAL SHORT AXIS (PSAX)
Once you have the PLAX view, rotate the probe indicator 90 degrees clockwise so it points to the patient’s left shoulder. You may need to tilt the probe inferolaterally to obtain a good view of the left ventricular apex (pictured) in the PSAX view. If you track superiorly, you will bring the mitral valve into view and then ultimately the aortic valve.
The best feature of the PSAX view is looking for left ventricular wall motion abnormalities. With one view, we can see all major coronary distributions (LCx – left circumflex, LAD – left anterior descending, RCA – right coronary artery) around the left ventricle’s walls (L – lateral, I – inferior, S – septal, A – anterior).
By viewing the video above, notice how the LV’s septal wall is hypokinetic. This regional wall motion abnormality could be due to pathology involving the septal perforating branches of the LAD. Cool clinical correlation. 🙂
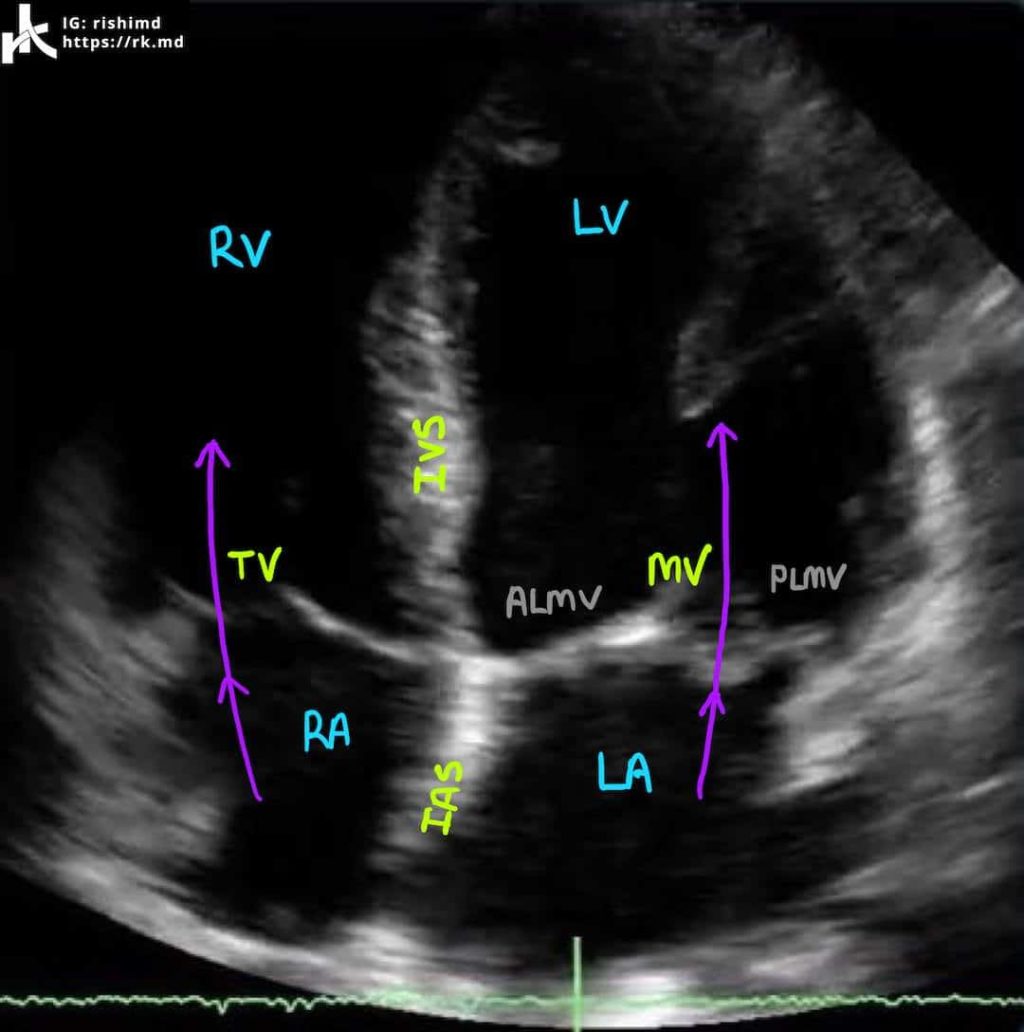
APICAL FOUR CHAMBER (A4C)
To obtain the apical four chamber (A4C) view, move the probe to the point of maximal impulse (usually just inferolateral to the left nipple) with the probe indicator pointed at 3 o’clock. I’ll usually have patients abduct their left arm to open up rib spaces. This view is great because blood flow across the mitral and tricuspid valves is parallel to the direction of the ultrasound beam allowing us to more accurately calculate gradients across the valves with doppler. We can also assess the size and function of all four chambers including and use other ultrasound techniques (M-mode) to crudely assess the right ventricle using TAPSE.
SUBCOSTAL FIVE CHAMBER
For the subcostal views, lay the patient completely supine. For the longitudinal view, place the probe below the xiphoid process with the indicator facing 3 o’clock. It takes a little pressure to direct the probe under the xiphoid in the direction of the heart. Be mindful that this can sometimes be uncomfortable for patients.
This view is often the only view which can be obtained during mechanical ventilation or with ongoing chest compressions. It can be used to assess for pericardial effusions, atrial/ventricular septal defects, and overall chamber size/function.
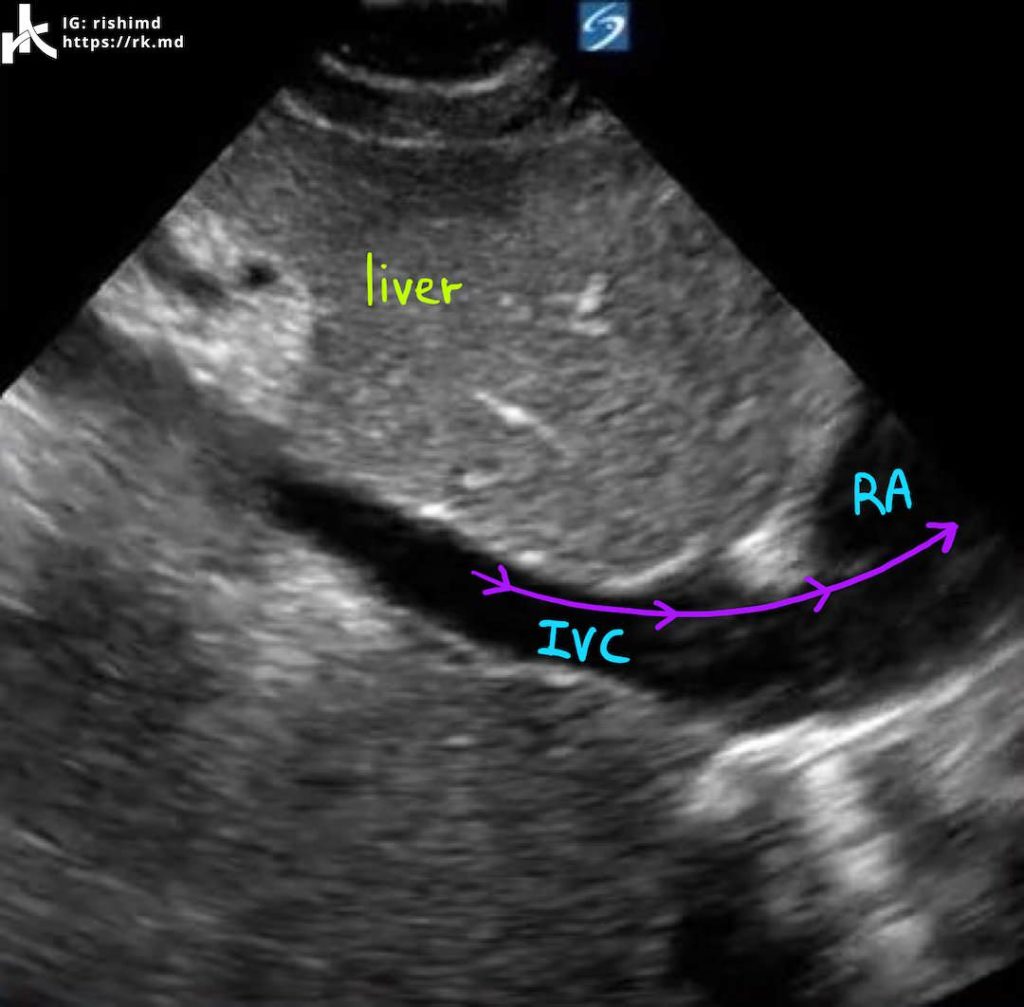
SUBCOSTAL INFERIOR VENA CAVA (IVC)
With the patient still supine, place the probe below the xiphoid with the indicator facing 12 o’clock (the patient’s head). Aim straight down into the abdomen and tilt superiorly to get a view of the IVC entering the right atrium.
Ensure that you are indeed viewing the IVC by tracking it into the RA and by seeing it join with hepatic veins. In this video, the structure is clearly the IVC as you can see a path directly into the heart. The aorta lives anatomically leftward of the IVC and both appear tubular on ultrasound, so differentiating the two is critical. Look for variation in the IVC’s diameter throughout the respiratory cycle. Large changes (> 50% change in diameter) may suggest intravascular volume depletion.
Hopefully this very basic primer is helpful! Drop me a comment below with questions! 🙂