With the number of patients receiving permanent pacemakers (PPMs) and implantable cardioverter-defibrillators (ICDs) increasing each year, we’ll see more of these devices in our respective clinical settings. With this post, I’ll try to simplify pacemaker nomenclature and discuss some of the considerations surrounding magnets and device settings.
All ICDs have a pacemaker function but NOT all pacemakers are ICDs. Most patients should carry cards with information about their device, but when it’s 2 AM and your patient is found down, a chest x-ray can help you determine the type of device (PPM vs AICD) based on where the pacer leads are located and the presence of a thicker defibrillating lead only found in ICDs. It’s important to know the patient’s underlying rhythm (ie, what do they do without their pacer) and the indication for the PPM/ICD in the first place. Also, all pacers have a minimum backup rate which is the threshold heart rate at which the pacer will kick in.
When in doubt or confused, call your friends in electrophysiology!
PACEMAKER NOMENCLATURE
Pacemaker nomenclature is most often written as a series of three letters (ie, VVI) but can be as much as five (DDDRO). I’m going to keep things simple! In order, the 3 or 5-letter nomenclature stands for:
- Chamber Paced: A (atrium), V (ventricle), D (dual)
- Chamber Sensed: A (atrium), V (ventricle), D (dual)
- Response to Sensed Beat: I (inhibit), T (trigger), D (dual), O (none)
- Rate Responsiveness: R (rate-responsive), O (none)
- Automatically increases the pacing (and cardiac output) to meet an increase in exertion
- Multisite Pacing: O (none), A (atrium), V (ventricle), D (dual)
For most of us, only the first three characters matter.
SINGLE CHAMBER
A single electrode is fed into either the right atrium (“A wire”) or right ventricle (“V wire”). Now let’s consider some basic nomenclature using the aforementioned patterns.
- AAI: The atrium is paced and sensed. If an intrinsic beat is detected (ie, the patient’s SA node fires), the pacemaker will inhibit itself. This makes sense in conditions like sick sinus syndrome (SSS) where the AV node is working fine and cardiac output can be maintained as long as the atria are firing at an appropriate rate.
- VVI: The ventricle is paced and sensed. If an intrinsic beat is detected (ie, conduction carried down through AV node into the ventricle), the pacemaker will inhibit itself. One can imagine that if the pacer has to constantly fire on the ventricle, some of the signal can be conducted retrograde into the atria during systole causing contraction against the closed tricuspid/mitral valves. Also, ventricular pacing causes the “atrial kick” to disappear which can have severe consequences in patients with poorly compliant ventricles requiring higher filling pressures.
DUAL-CHAMBER
A wire is fed into the right atrium AND right ventricle. DDD is the most common mode I work with. In this setting, the pacemaker can independently sense and pace one or both of the chambers. Because of this, the patient’s EKG can show several rhythms:
- Sinus rhythm: The patient’s native heart rate is faster than the backup rate of the pacemaker. There is normal atrioventricular conduction.
- A sensed, V paced
- A paced, V sensed
- AV pacing: both chambers are paced
Now let’s briefly discuss pacemaker mode switching. If a patient with a DDD dual chamber pacemaker suddenly develops an atrial tachyarrhythmia (atrial rates can exceed 500 bpm), it doesn’t make sense for the pacemaker to fire the ventricle at that rate. Instead, it’ll detect the fast atrial activity and “switch” into a safer mode (like VVI) to basically ignore atrial activity.
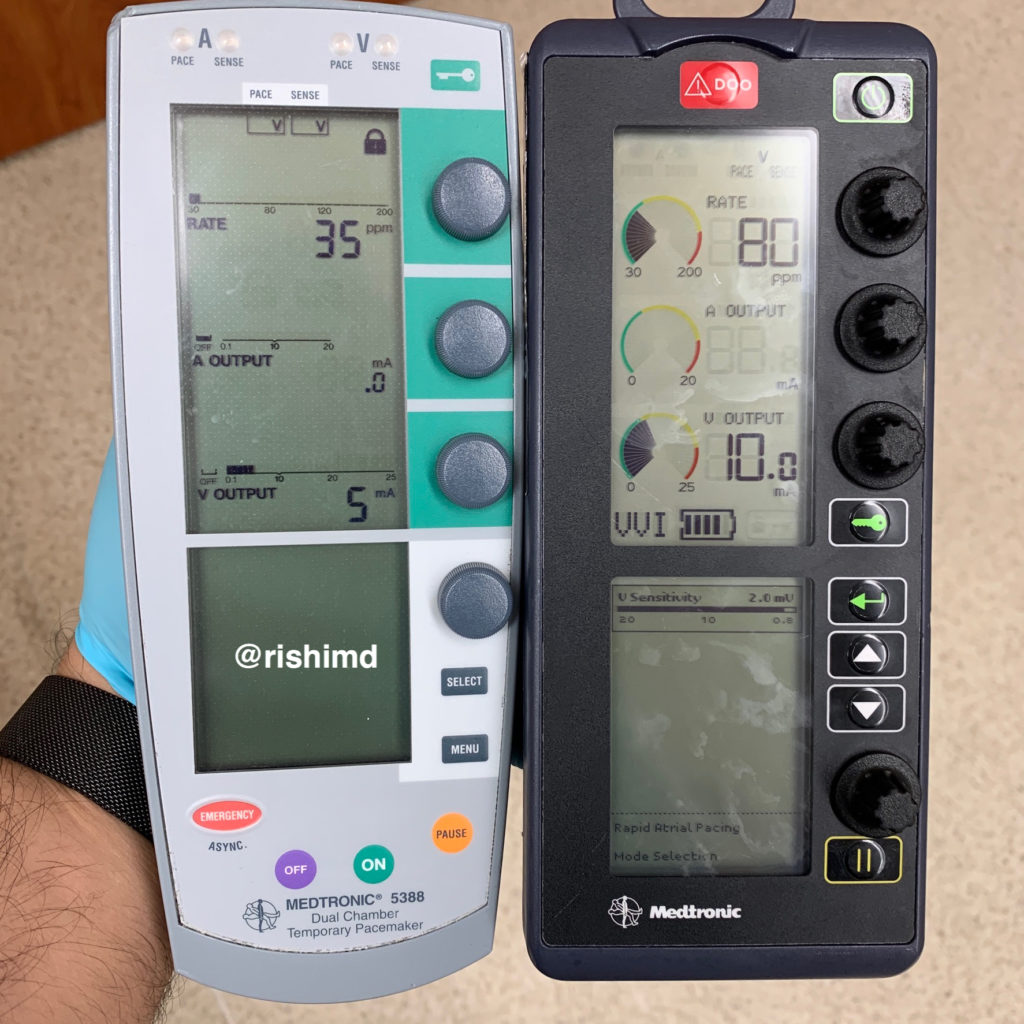
PACEMAKER SETTINGS
The purpose of temporary pacemakers is to sense intrinsic electrical activity and pace the myocardium from the inside (ie, transvenous wires) or outside (epicardial wires). Following cardiac surgery, surgeons often place bipolar leads on the right ventricle (RV) for ventricular sensing/pacing +/- right atrial (RA) leads for synchronized atrioventricular pacing. A current is delivered between the two bipolar leads and “captured” by the myocardium resulting in depolarization.
There are three major settings for pacers:
- Rate: the number of impulses/minute
- Output (mA): the current needed for the myocardium to “capture” the paced signal. In other words, how energy much are you jolting the heart with. Atrial output and ventricular output range from 0.1 – 20 mA and 0.1 – 25 mA, respectively.
- Sensitivity (mV): the point at which the pacing device interprets a native myocardial signal as a pulse. The greater the millivolts, the less sensitive the device is to native cardiac activity which can lead to undersensing and overpacing potentially causing the pacer to fire on a native heartbeat (R-on-T phenomenon). At higher sensitivities (lower millivolts), any – little – signal (including breathing, patient movement, etc.) will be interpreted as a native beat (oversensing).
To “test” a pacer, I select a mode (typically DDD for A-V pacing wires and VVI for only V pacing). I’ll start with the default output and sensitivity settings and increase the pacer rate to something above the patient’s native heart rate. Then I’ll watch the continuous EKG to ensure that the signal is indeed captured at the preset rate while dialing down the output.
If a pacer loses its ability to capture, one must consider possible changes in sensitivity thresholds, electrolyte changes, damaged lead(s), battery depletion, or faulty cables. If I seem to have competition between the pacer and the patient’s native heart rate, I’ll adjust the sensitivity to avoid the aforementioned scenarios of over/undersensing.
ICDs
Implantable cardioverter-defibrillators (ICDs) are placed for a myriad of reasons ranging from low ejection fraction states and sustained ventricular tachycardia/fibrillation to prior cardiac arrest from channelopathies or structural heart issues like hypertrophic cardiomyopathy. Remember, ALL ICDs have an intrinsic pacemaker function. The question is whether or not the patient is truly “pacer dependent.” This is where recent interrogation reports are important.
MAGNET
Keeping it simple: a magnet will reprogram a regular pacemaker into an asynchronous mode (AOO, VOO, DOO) at a manufacturer-defined heart rate. By contrast, a magnet will deactivate an ICD’s “shock” function; however, the pacemaker portion of the ICD will not be changed.
This is the question I’m often asked as a cardiothoracic anesthesiologist and intensivist.
“Rishi, I have a patient with (insert device name here)… do I need to put a magnet on?”
My first questions are:
- Why does the patient have the device?
- Is the patient “pacer dependent?”
- What’s the surgery? Is electrocautery involved? Are the surgeons working near the chest?
In my specialty, the most common situation I run into is a patient with an ICD coming in for cardiothoracic surgery. The device is located in the surgical field and, oftentimes, will be explanted (ie, at the end of a heart transplant). As mentioned above, a sterile magnet will disable the ICD’s shock function but not affect the pacemaker function. If the patient is also pacer dependent, electrocautery in the field can be misinterpreted as intrinsic cardiac conduction system activity. The pacemaker portion will think the patient’s heart is firing on its own (when in reality, it’s the electrocautery), and the device will therefore inhibit itself. Now the patient’s true heart rate will become apparent which can significantly drop the cardiac output leading to bradycardia/bradyarrhythmias and hypotension.
If you feel like this is a potential scenario in your situation, the safest option is to have the electrophysiology team come reprogram the device to an asynchronous mode prior to surgery. Although I usually also place external defibrillator pads on these patients, remember that if they go into a “shockable rhythm” intraoperatively (ie, VFib), just remove the magnet and let the ICD function kick in.
Lots of information covered in this post – please drop me a comment below with questions!







I put a magnet on an icd and the pacemaker started to pace my patients heart at 100 bpm. Any idea why it would do that?
Not sure. What was the make/model of the device?
Eh sorry I don’t really remember. I think Abbott was the brand though.
Fantabulous Article
Do you need to put a magnet over AICD during Ercp
As I stated in the post, whenever someone asks me this question, they also need to know the answers to the following questions: Why does the patient have the device? Are they “pacer-dependent?” Is electrocautery involved?
In most cases, although the magnet will deactivate the “shock” function in most cases, it won’t do anything to the pacing function. If the patient is pacer dependent and electrocautery is misinterpreted as native cardiac electrical activity, profound bradycardia may result.
Do you have a rule of thumb as to when you do and don’t place a magnet? For example, if cautery is to be used below the umbilicus and above the chin, will you place a magnet? Also, when should a magnet be placed over a PPM?
I’ll place a magnet over a pacemaker if a patient is pacemaker dependent, and I’m even remotely concerned about interference from electrocautery being misinterpreted as endogenous electrical activity. If a path from the operative site to the grounding pad can cross paths with the device, then I’ll either reposition the grounding pad or place a magnet to convert the pacer to an asynchronous mode.
Great! Thank you for your feedback.
Without interrogation, how can you be sure that a pacemaker’s magnet response has not been reprogrammed? I believe reprogramming magnet response is possible on all manufacturers devices except Medtronic. Also, how can you be certain that the magnet placement on an ICD is correct and remains correct?
I’m not sure how to know with certainty. As far as if the magnet is doing its job on an ICD – some devices have an audible beep for feedback.
What do you think of magnets on prone lumbar surgery patients? The cautery is in low back area. But, I worry about laying on a magnet for up to several hours. Could external pacer/defib pads cover any issue if needed?
Excellent question, Stacy! Honestly, if I was doing this case and I was concerned about pacemaker dependence, I would get the electrophysiology team to reprogram the pacer/ICD. External defibrillator pads should work just fine.
Does bipolar make any difference about placing or not placing a magnet. Also if a magnet is placed is it appropriate to have the device checked prior to discharge?
Great questions! Theoretically, bipolar electrocautery should keep the electrical current isolated within a small area (between the two points of the electrocautery device); however, especially if working near the ICD/pacemaker, I wouldn’t be 100% comfortable banking on this if my patient is pacemaker dependent.
As far as device interrogation prior to discharge, I don’t think it’s necessary unless there’s a concern (ie, an ICD unexpectedly fired intraoperatively). I’m sure some institutions have protocols regarding this, but this is just my opinion.