An important aspect of understanding mechanical ventilation is knowing how to interpret peak inspiratory pressures (Ppeak) and plateau pressures (Pplat). What’s the difference, and why does it even matter?
Think of the ventilator, inspiratory limb tubing, endotracheal tube, and your patient’s airway as a long, continuous pipe with a diameter much smaller than the overall length. Poiseuille’slaw shows that the resistance (‘R’) in this “airway pipe” is directly related to the length of the pipe and indirectly related to the radius raised to the 4th power. In other words: R ~ length / radius4. For example, if the radius of the pipe is cut in half, the resistance increases by a factor of 16.
What can cause this “pipe” to be narrowed? What if the tubing leaving the ventilator is kinked? What if the patient is biting the endotracheal tube? What if the airway lumen is reduced because of bronchospasm or mucous plugs? These will all effectively increase airway resistance to varying degrees… but how does this affect the peak and plateau pressures?
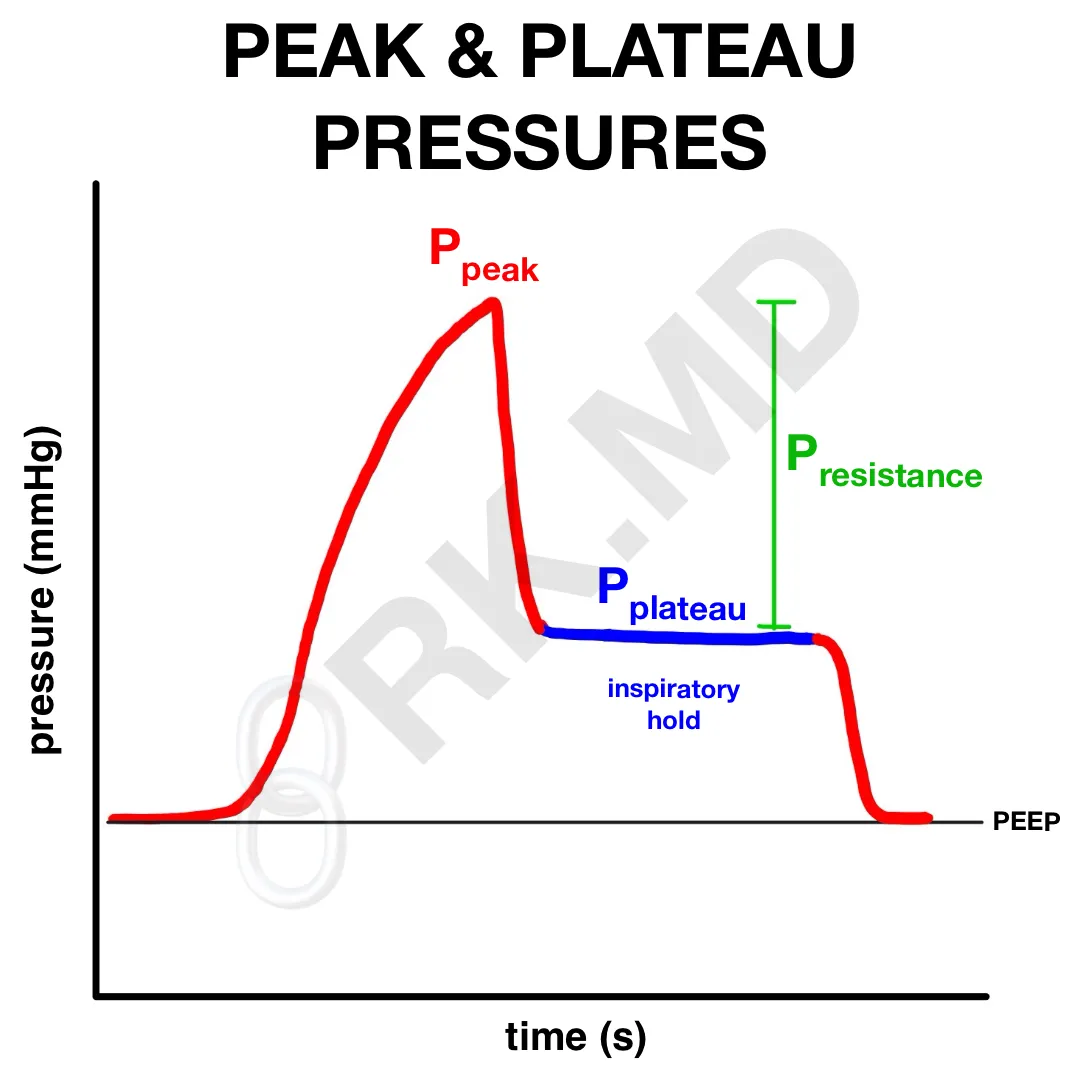
During an inspiratory hold maneuver, a fixed volume of air is delivered into the lungs. Ppeak is determined at the end of that inspiration. This breath is then held in (ie, the patient is not allowed to exhale). During this time, the airway pressure drops to a new level – the plateau pressure (Pplat). The drop-off is the pressure required to overcome resistive forces (Presistance) such as chest wall/lung elastic recoil and friction during inspiration. In other words: Ppeak = Pplat + Presistance
Now how does this translate to a real-world example? Let’s say you walk into the room and see a Ppeak of 60 cm H2O (normal is 25-30 cm H2O). Pplat is only 20 cm H2O during the inspiratory hold. That means there’s a huge pressure overcoming airway resistance (ie, a very high Presistance)! Now I’m thinking more about things that are decreasing the radius of the airway pipe. For example, narrowing of the endotracheal tube, mucous plugs, and circuit kinks could be causes.
What if the Ppeak was 50 cm H2O and the Pplat was 45 cm H2O? The high Pplat points towards a lung issue affecting the lung itself such as decreased pulmonary compliance, edema, pneumothorax, or evolving parenchymal disease like pneumonia or ILD.
Drop me a comment below with questions! 🙂






What does it mean if your PPLAT And PIP are close together or less than 5cm apart ? For example a pplat 20 and PIP of 22?
I’ve always understood that if they are close together that the lung is tight but is that the same with such a low number ?
Thank you
If they’re roughly the same, there’s unlikely to be much intrinsic airway resistance (mucous plugs, kinked circuit, bronchospasm, etc.). If the peak/plateaus are both high, then I’m considering situations like decreased pulmonary compliance, edema, pneumothorax, or evolving parenchymal disease like pneumonia or ILD.
This was wonderfully explained. I was scared when you started with physics but you did it in a great way and i feel so much more comfortable!
Thanks for the feedback! 🙂
Dr. Rishi, thank you for this concise, clear explanation of things. PIP must always be greater than plateau pressure. If something affects airway resistance alone (narrowed airway lumen), then the difference between PIP and PEEP will increase. If something affects the compliance of the alveoli alone, raising plateau pressure, does that always raise the PIP? If so, does it raise it by the same amount, assuming that airway resistance stays the same?
Ex: PIP 30 cm H2O with P-Plateau 20 cm H2O. If we increase the P-Plateau to 25 cm H2O, does PIP increase to 35 cm H2O with it, does PIP remain at 30, or is there a different relationship?
Hey Stephen, please just call me Rishi! I wouldn’t assume that changes in Pplat or Presistance occur in isolation. For example, let’s say a patient has worsening pulmonary edema. Their lung compliance will worsen (increasing Pplat) but perhaps their airway secretions may worsen as well (for the same reason) causing an increase in the PIP higher than an increase in Pplat alone would explain.
At the end of the day, we just check peak and plateau pressures.
Nicely explained, thanks.
Excellent sr… I understood.. I do critical care technology lll yr . if I have doubts , I’ll ask you sr..
Can small ETT tube increase plateau pressure in adults patients?
More likely to increase peak pressures with minimal effect on plateau.
what is the relation of peak and plateau once the patient position is changed, like putting in prone with the patient on PCV mode of ventilation? Do they still remain the same?
They don’t necessarily remain the same.
Hi Rishi!
I am an anesthesiologist assistant student and I wanted to know what kinds of interventions you could perform in a ventilated patient who has high peak airway pressures? What settings could you adjust to fix this?
Hey Alexandra! So first thing you want to do is rule out any “easy fixes” like mainstem intubation, mucous plugging, and possibly bronchospasm (low dose epinephrine/ketamine, deepening the anesthetic, etc.). Next, you could optimize the actual ventilator parameters by adjusting the I:E ratio (sometimes patients need more expiratory time), decreasing tidal volume a bit (and going up on respiratory rate to maintain minute ventilation), increasing PEEP (which sounds like it’ll increase overall airway pressure, but sometimes you’ll actually see a decrease in the mean airway pressure since less inspiratory pressure is required to open the alveoli each time), or changing your overall mode to something like auto flow.
Is there any relationship between the duration of pause period and plateau pressure? For example, will a longer inspiratory pause period result in lower plateau pressure?
It shouldn’t make a difference.
Does a high respiratory rate affect obtaining a plateau pressure? For example, if I have a patient on volume control with a RR: 34 and I change the inspiratory time to 50% to perform an inspiratory hold on an anesthesia machine will I get an accurate plateau pressure?
I’ve not actually done this manually on an anesthesia ventilator (it usually calculates this periodically on its own). A true inspiratory hold maneuver is just that – a transient hold. There’s no adjusting I:E ratio or anything. Most ICU ventilators will have an option to perform this maneuver, and as long as the patient doesn’t have any spontaneous inspiratory effort and there’s no circuit leak, it should be fine.
Thanks Rishi! We are using many of our anesthesia machines as vents for our COVID+ patients in our makeshift ICUs, so getting a plateau pressure has been an adventure.
wonderful attempt. very much useful. But approach is much useful
Thank you!
Beautifully explained. looking forward to read more such articles. Keep up the good work.
Thank you so much! 🙂
Thank you for this simple explanation.. never saw it in this way .. will pass it on to my juniors!
Glad I can help! Let me know if you (or your juniors) have questions! 🙂
Thanks for this. I am very happy if u will write mu email.
No problem! 🙂
This is awesome—I especially appreciate your ability to write in a way that’s conversational and framed in simple (read: clerkship student-friendly) terms. Thanks!
Thanks Amol! I aim to write in simple terms so everyone, regardless of trainee level, can understand more complex concepts. Hope you’ve been well bro! 🙂