Often times we hyperventilate patients in the operating room with the justification that a low PaCO2 will suppress a patient’s desire to take spontaneous breaths during surgery (ie, less of a chance the patient will “move”). While there is some merit behind this (the hypercarbic drive), I assure you that volatile anesthetics, narcotics, and neuromuscular blockers will also help with immobility.
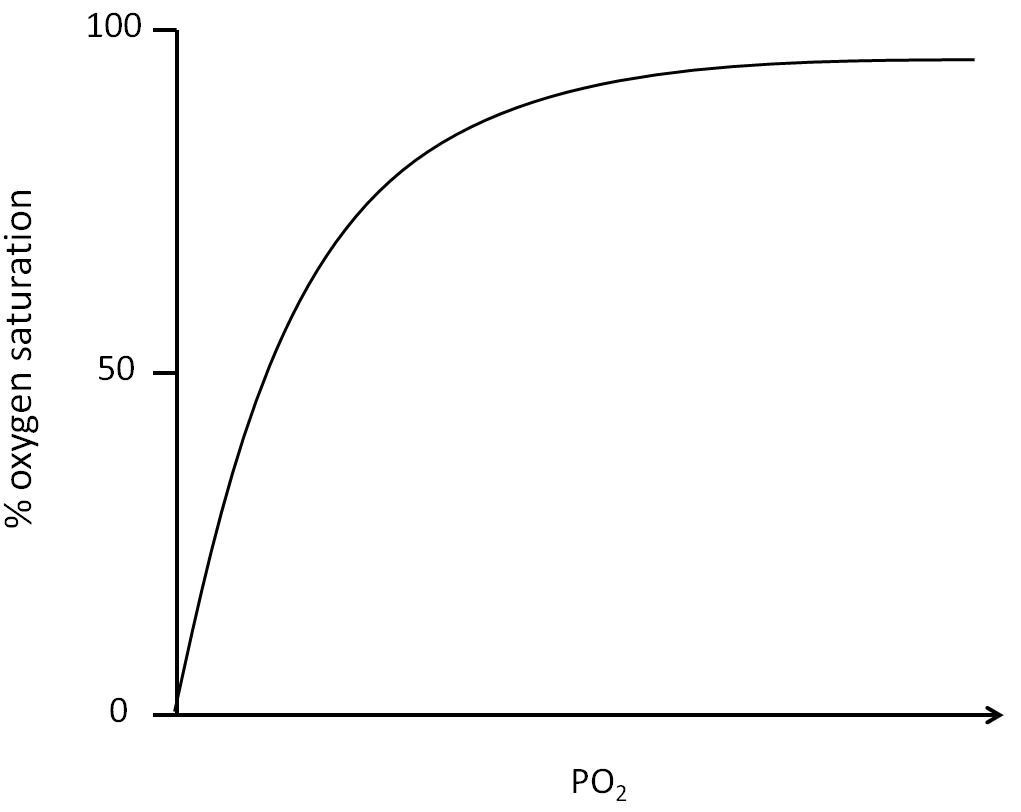
Acute hyperventilation will result in an acute respiratory alkalosis and cause a leftward shift in the oxyhemoglobin dissociation curve – termed the Bohr Effect. This physiologic change is characterized by increased binding of oxygen to hemoglobin. Although your pulse oximeter hemoglobin saturation might be reassuring, keep in mind that the Bohr Effect also means there is reduced oxygen delivery to the end organs and tissues. In other words, while oxygen is better able to bind hemoglobin, the hemoglobin molecule is less willing to unload oxygen at the tissue level. Tissue hypoperfusion = ischemia = bad. 🙁
I make it a point to only have a slight drop in my patients’ baseline PaCO2 while under general anesthesia. Since we’re not checking blood gases during every gas, our continuous capnogram’s end-tidal CO2 serves as a surrogate marker for ventilation. We often have full control over our patients’ respiratory function in the operating room – be mindful of the systemic changes you can create.