It’s important for me to consider the surgical steps and potential areas of difficulty/complications which may arise intraoperatively. Although each procedure must be tailored to a patient’s unique set of comorbidities and surgical factors, I wanted to outline the basic steps involved in routine coronary artery bypass grafting (CABG).
First, a median sternotomy is made using a pneumatic saw (“cracking the chest”). The left internal mammary artery (LIMA) is dissected off the chest wall while an assistant usually performs ultrasound mapping of the saphenous vein system and harvests saphenous vein grafts from the legs endoscopically or with an open incision. Intravenous heparin (usually 4 mg/kg) is administered as the pericardial sac is opened. The remainder of the LIMA dissection is performed and the vessel is clamped distally.
Next, the ascending aorta is cannulated through two purse-string sutures. At this point, it’s possible to begin cardiopulmonary bypass (CPB) as long as sufficient volume is provided from the bypass reservoir. A venous cannula is inserted through two purse-string sutures into the right atrial appendage. By doing this, blood is drained from the right atrium into the CPB reservoir, then sent through a pump/oxygenator, and ultimately circulates back to the aortic return cannula. Once bypass is initiated, an ascending aorta cross-clamp is placed.
If the heart is going to be “bloodless” to facilitate surgery, we better make sure its demand for oxygen is also minimal. This is achieved through a diastolic arrest with high potassium cardioplegia solution. An antegrade cardioplegia catheter is placed into the aortic root to deliver the cardioplegia solution directly down the coronaries in the same way blood normally fills this network. A retrograde catheter is sometimes placed into the coronary sinus to fill the coronary network backward. Additionally, the heart is topically cooled with ice slurry. The combination of cooling the heart, emptying it with bypass/venting to decrease wall stress, and arresting it with cardioplegia helps mitigate the mismatch between oxygen supply and demand after the aortic cross-clamp makes the heart ischemic.
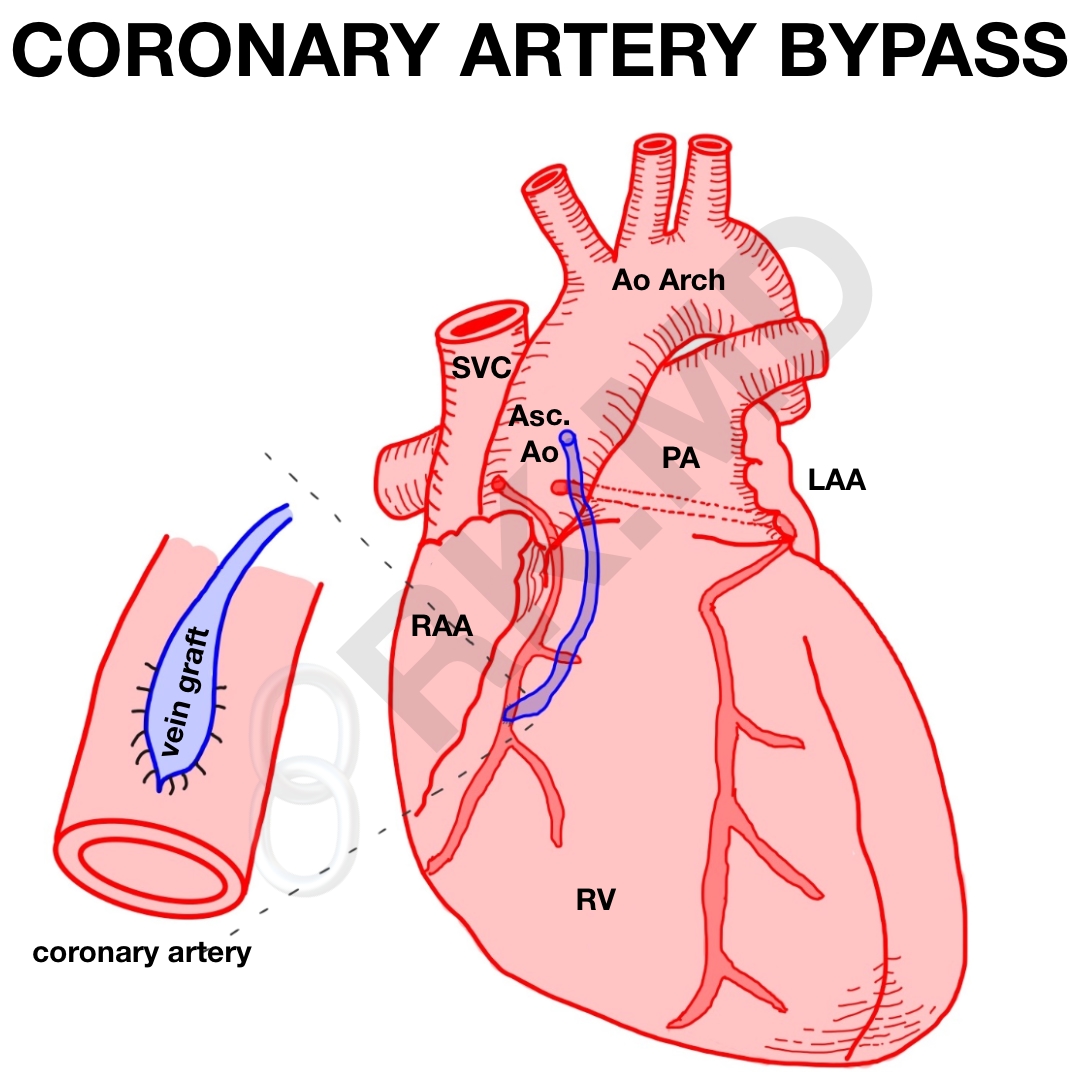
Next, vessel grafting commences. The posterior, distal grafts (e.g., right coronary artery) are performed first. Reversed saphenous vein grafts (SVGs) are anastomosed end-to-side distal to the diseased coronary artery in a running fashion. Since the LIMA is already connected to the aorta proximally and the left anterior descending (LAD) coronary artery is on the anterior heart, the LIMA-LAD end-to-side distal anastomosis is usually done last.
All the vein grafts now need to have their proximal anastomoses completed onto the ascending aorta in an end-to-side fashion. Systemic rewarming is initiated and a partial occluding clamp is placed on the aorta prior to beginning these proximal anastomoses. Once finished, de-airing is performed of all the grafts and right ventricular pacing wire is placed.
Weaning from cardiopulmonary bypass is its own topic but requires careful coordination between the surgeon, anesthesiologist, and perfusionist. Transesophageal echocardiography (TEE) is especially useful at this point to guide weaning. Once successfully weaned, the bypass cannulas are removed and systemic heparinization is reversed with protamine sulfate. Chest tubes are left in the mediastinum and left pleural space. The sternum is closed with stainless steel wires, and the overlying fascial layers are closed with absorbable sutures.
Drop me a comment with questions! 🙂







Hi! I am writing a PCCN course for nursing.com and have found this incredibly helpful! Thank you!
You’re welcome!
This was so helpful, thorough, and well-explained. Please do more of these, maybe describing aortic and valve surgeries. Thanks!!!
Glad you found it useful! 🙂
Hi- What sutures are typically used and where? I’m a scrub tech student doing my case summaries and that is one of the questions.
Not sure. There’s also some variability among surgeons.
Just wanted to say thank you for this blog post. I just started a surgical residency as a physician assistant and I’m currently in CT surgery. Felt like this was a nice explanation that helped a lot. Really appreciate your posts.
So glad you found this helpful! Thanks for taking the time to write such a nice comment! 🙂
Hi, thanks for these steps! It would be cool to have a detailed article with each step to a CABG and the corresponding anesthetic action and what could go wrong (and anesthetic response to this).
Hey Vivi, I’ll think about it, but honestly there are just too many combinations of things I look at to really do justice to the clinical decision-making with a blog post. ????????♂️
it’s 1:26 am on a saturday.
PACU is calm.
I am reading some quality posts by Dr. Kumar.
This is living.
Hahaha, thanks Dr. Luo! I’m seriously going to miss you man. Best of luck finishing the last few days of residency!