Amiodarone (Pacerone) is an antiarrhythmic that works by prolonging the myocardium’s refractory period through potassium channel, sodium channel, calcium channel, and beta-blockade. Its side effects can be remembered by their effects on “PFTs, TFTs, and LFTs” (pulmonary, thyroid, and liver testing, respectively) in addition to corneal, neurological, and skin changes.
Hypotension from amiodarone is actually more likely due to solvents that the medication is dissolved in (polysorbate or benzyl alcohol). Some case reports cite using lipid emulsion as a rescue, but eh, I’m just careful with boluses.
The FDA approved amiodarone for recurrent ventricular fibrillation (VFib) or refractory ventricular tachycardia (VTach). Notice that I did NOT say atrial fibrillation. We use amiodarone off-label for this purpose.
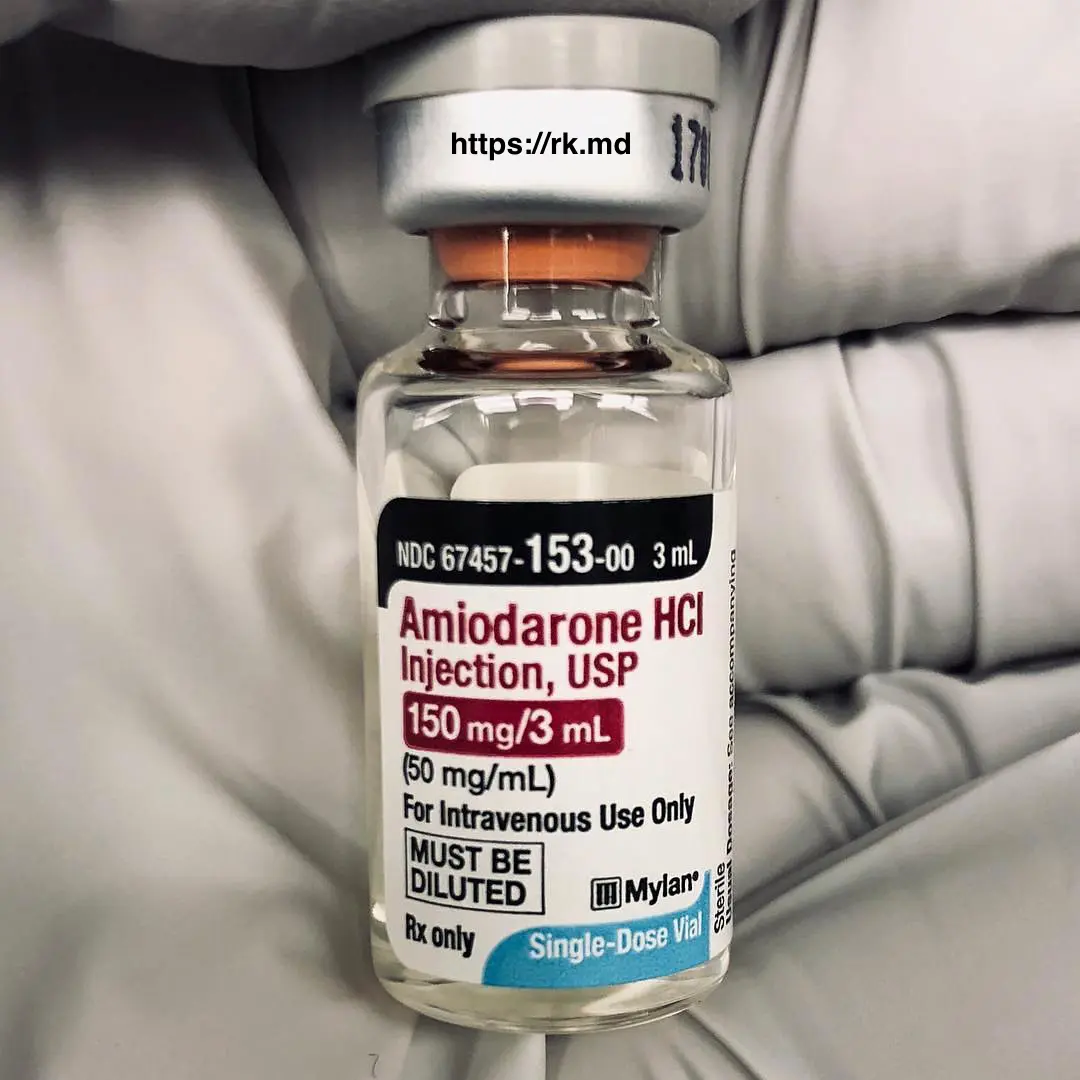
Amiodarone should ideally be administered through a microfilter (to catch precipitants) and through a central line or rotated through peripheral IVs due to its vesicant properties (pH ~ 4). Sometimes I give a 150-300 mg load in the OR coming off cardiopulmonary bypass. In the ICU, I’ll write for a slow bolus of 150 mg followed by 1 mg/min for 6 hours and 0.5 mg/min for 18 hours. Occasionally I’ll bolus on top of the infusion not to exceed 2.2 grams in a 24 hour period. In any case, amiodarone has a long half-life, so I’m stuck with the consequences.
Drop me a comment below with questions! 🙂






Is amio efficacious for SVT?
Haven’t used it for that. I stick to calcium channel blockers or adenosine.
Is this amio bolus upon bypass weaning/removal prophylactic in nature due to the high occurrence of atrial tachs that most procedures requiring bypass suffer from or due to intraop rhythm changes?
Hey Jake, most often, it’s for prophylaxis and/or treating arrhythmias coming off of bypass.