For the last several months, multiple manufacturing delays have led to a nationwide shortage of injectable, intravenous (IV) opioid medications like morphine, hydromorphone, and fentanyl. These medications are routinely utilized in the perioperative and intensive care settings for analgesia and sedation, so the shortage has forced us to incorporate other modalities to achieve the same goal. Coming from an anesthesiology background, I have always been an advocate for multimodal analgesia. Now is the time for all disciplines to learn that there are other ways to control pain besides morphine 2-4 mg IV q4h PRN for pain. Here are some ways I manage pain in the ICU in the context of an ongoing IV opioid shortage.
OPIOIDS
Huh? Didn’t you say there was a shortage? Yes – intravenous opioids.
Opioids like PO morphine, PO hydromorphone, and PO oxycodone are still widely available. I’m a firm believer that opioids are a good modality for pain control and have a role in multimodal analgesia… especially immediately post-op. In general, if I have access to the gut, I’ll use it. Here are some examples:
- oxycodone 5 – 10 mg PO q3h PRN for pain
- hydromorphone 2 – 4 mg PO q3h PRN for pain
REGIONAL TECHNIQUES
Regional and neuraxial anesthesia techniques are incredibly versatile! Depending on the type of surgery, contraindications, and expected post-operative course, I may push for an epidural to be placed for my operative patients and even trauma patients who come to the ICU. Other options include peripheral nerve blocks (PNBs). Using ultrasound, we delivery an infusion of local anesthetic medication via catheters near nerve bundles or within muscles planes to provide a targeted form of analgesia.
NON-NARCOTIC INFUSIONS
The frequency of monitoring in the ICU makes titrating medications much more feasible. Here are some IV infusions I frequently use:
- lidocaine IV infusion at 0.5 – 2.0 mg/kg/hr
- ketamine IV infusion at 1 – 5 mcg/kg/min
- dexmedetomidine IV infusion at 0.2 – 1.4 mcg/kg/hr
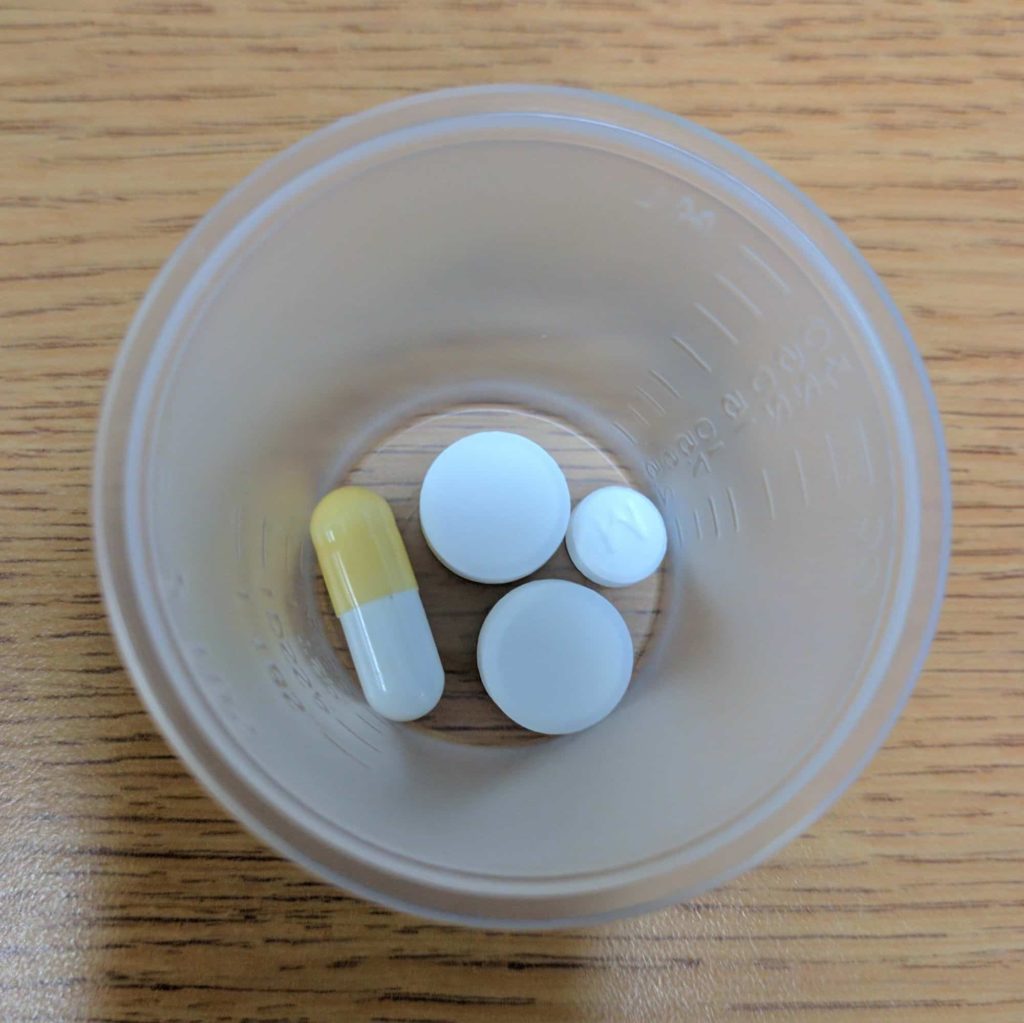
ADJUNCTS
True to multimodal analgesia, let’s attack pain through different mechanisms! Here are other common medications I utilize:
- ketorolac 15 mg IV q6h scheduled or ibuprofen 800 mg PO q6h scheduled
- acetaminophen 1000 mg PO/IV q6h scheduled
- gabapentin 300-600 mg PO q8h scheduled
- methocarbamol 1500 mg PO TID/QID PRN
- clonidine 0.1 – 0.3 mg PO q8h scheduled
- Lidoderm patches
- Heat/cold therapy
How about an example?
For certain thoracic and abdominal procedures, I’ll plan for a low-mid thoracic epidural running 0.1% ropivacaine with 2 mcg/cc of fentanyl which I’ll begin running fairly early in the case (6-10 cc/hr). I’ll also drop an orogastric tube but won’t suction until at least one hour has passed after administering 1000 mg PO acetaminophen, 200 mg PO celecoxib, and 300 mg PO gabapentin pre-operatively.
The surgeons will infiltrate local anesthetic with the surgical incision, and I’ll use adjuncts like ketamine (0.5 mg/kg at incision, 0.2 mg/kg every hour), dexamethasone (4-8 mg IVP), and ketorolac (15 mg q6h IVP) to supplement the epidural analgesia. If the epidural just doesn’t seem to be doing the job, I’ll add a lidocaine drip (2 mg/kg/hr) with low-dose dexmedetomidine (0.3 mcg/kg/hr) or even consider transversus abdominis plane (TAP) and PECS I/II peripheral nerve blocks. Throughout the case, I’m also constantly repositioning the neck/shoulders/head/limbs and considering all potential areas of nerve stretching or pressure injuries.
Yes, this seems like polypharmacy, but each of these medications has a particular role in modulating the pain cascade. Obviously the regimen is tailored for a patient’s comorbidities and the nature of their surgery, but the aforementioned are just some of the techniques I routinely use.