Phenylephrine is a selective α1 receptor agonist used in various settings for its vasoconstrictive properties. Whether this is as a decongestant (constricting vessels in the nasal/sinus mucosa) or a mydriatic to perform a fundoscopic exam, this medication’s selectivity gives me an idea of the expected response and potential side effects.
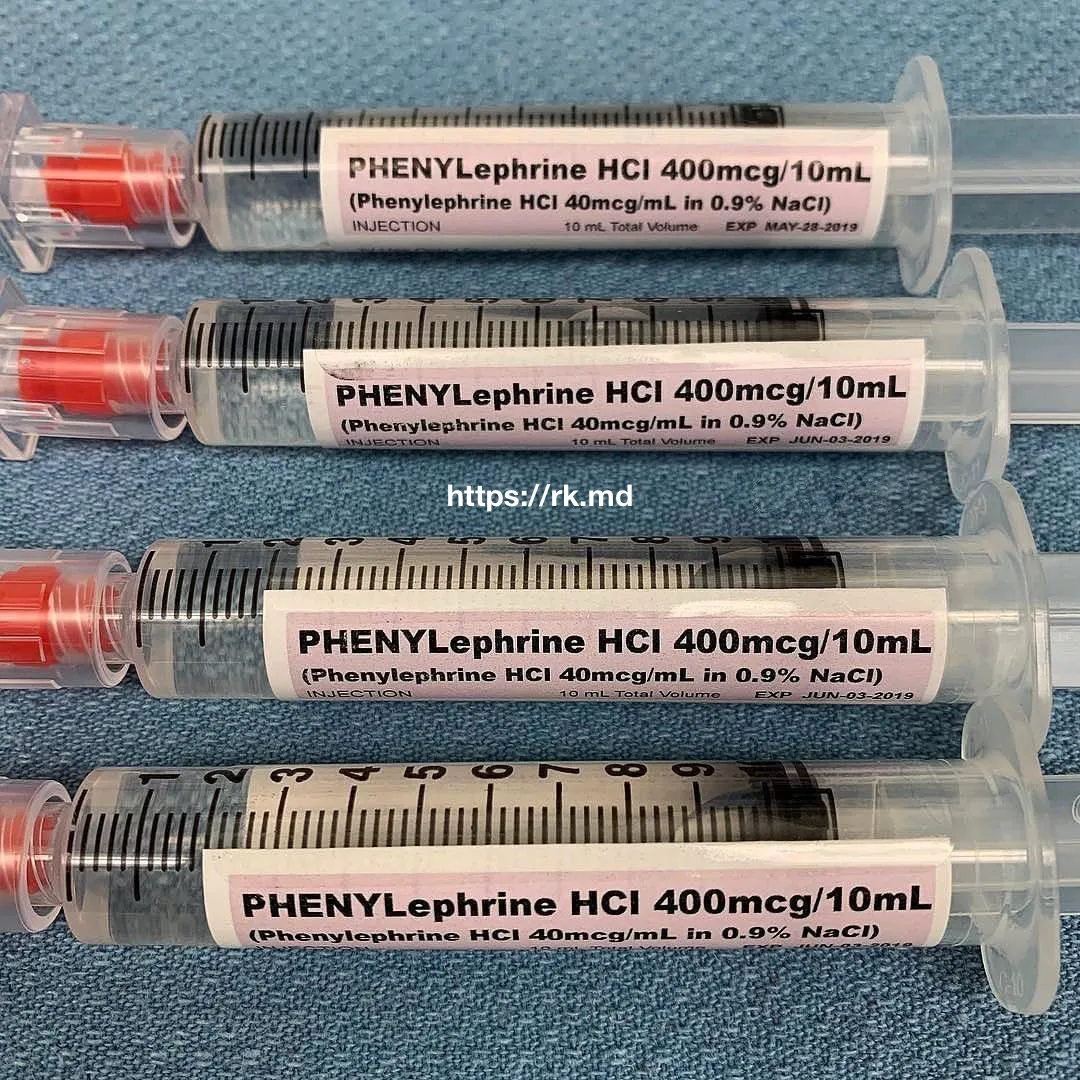
I most commonly use phenylephrine in the ICU and OR to treat acute hypotension caused by vasodilation from hypnotics, halogenated volatile anesthetics, or acute blood loss in tandem with ongoing resuscitation. I’m comfortable using a peripheral IV to bolus 40-120 mcg quickly. Still, in the rare event of tissue infiltration, phenylephrine’s alpha-agonist effects can be antagonized with medications like phentolamine administered subcutaneously. If the need for long-term afterload enhancement arises, I almost always switch to a norepinephrine or vasopressin drip.
Acute increases in systemic vascular resistance (SVR) will activate baroreceptors (i.e., the carotid sinuses), which, in turn, increase vagal tone to the heart. Since phenylephrine has no β-agonist properties, the unopposed increase in vagal tone is the mechanism by which the patient’s heart rate decreases in response to an acutely elevated SVR.
Drop me a comment below with questions! 🙂