Blood conservation strategies are routinely utilized in cardiac surgery with the aim of reducing the overall need for transfusions. Things like Cell Saver, retrograde autologous priming (RAP) of the cardiopulmonary bypass (CPB) circuit, using CPB tubing that requires less priming, and intraoperative autologous blood donation (IAD) with isolation of platelet rich plasma (PRP) are all techniques I’ve used in my practice.
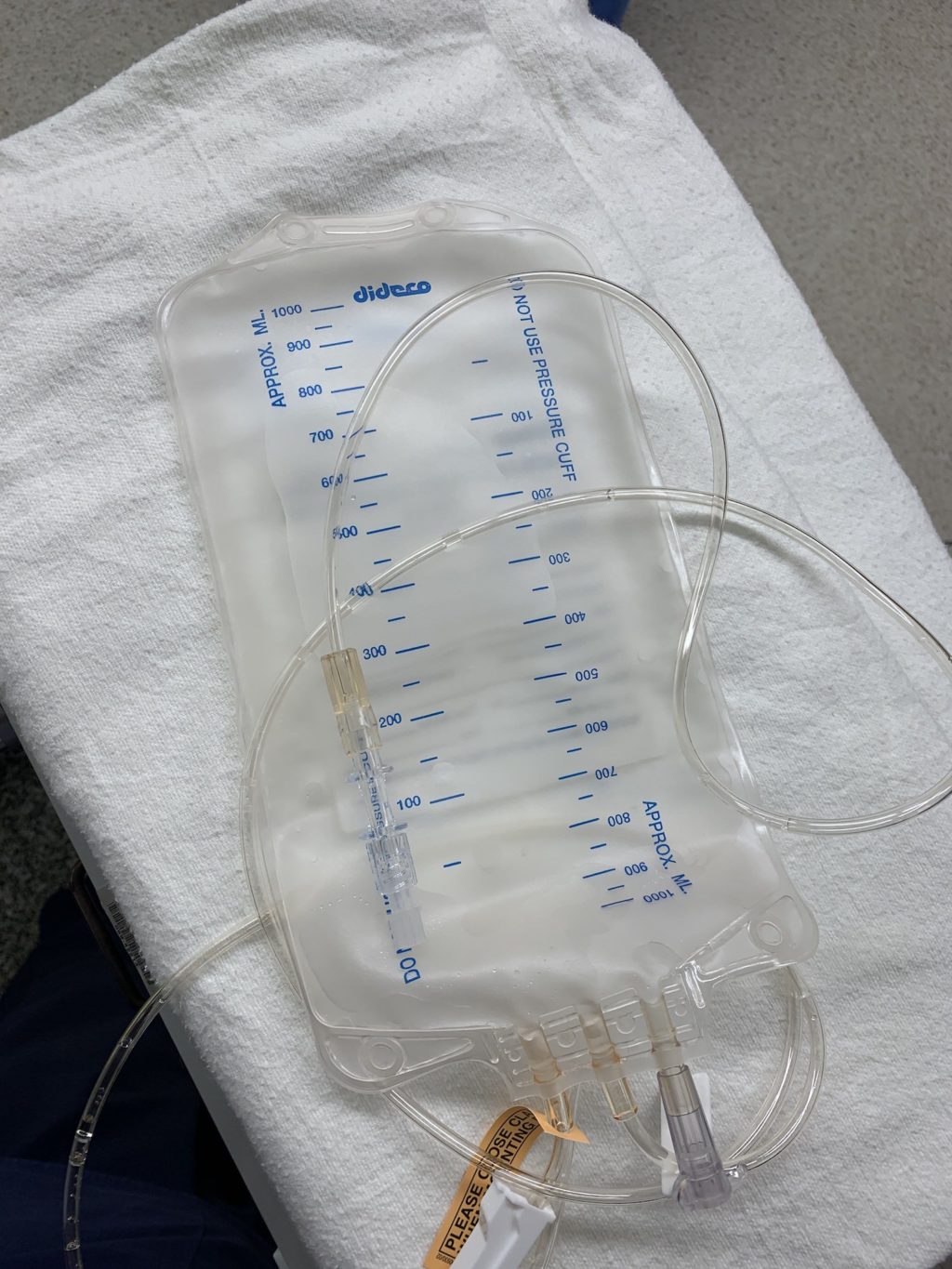
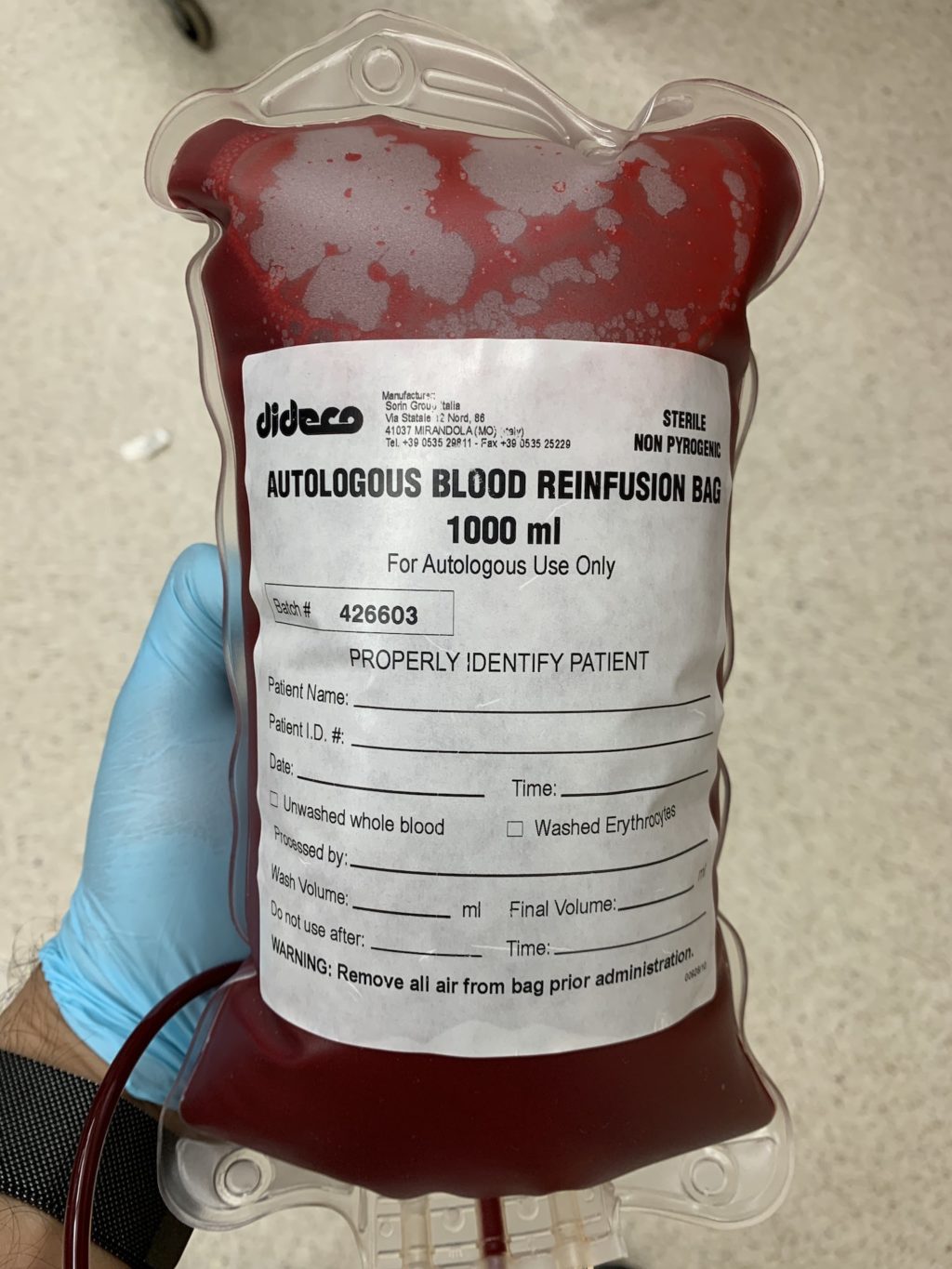
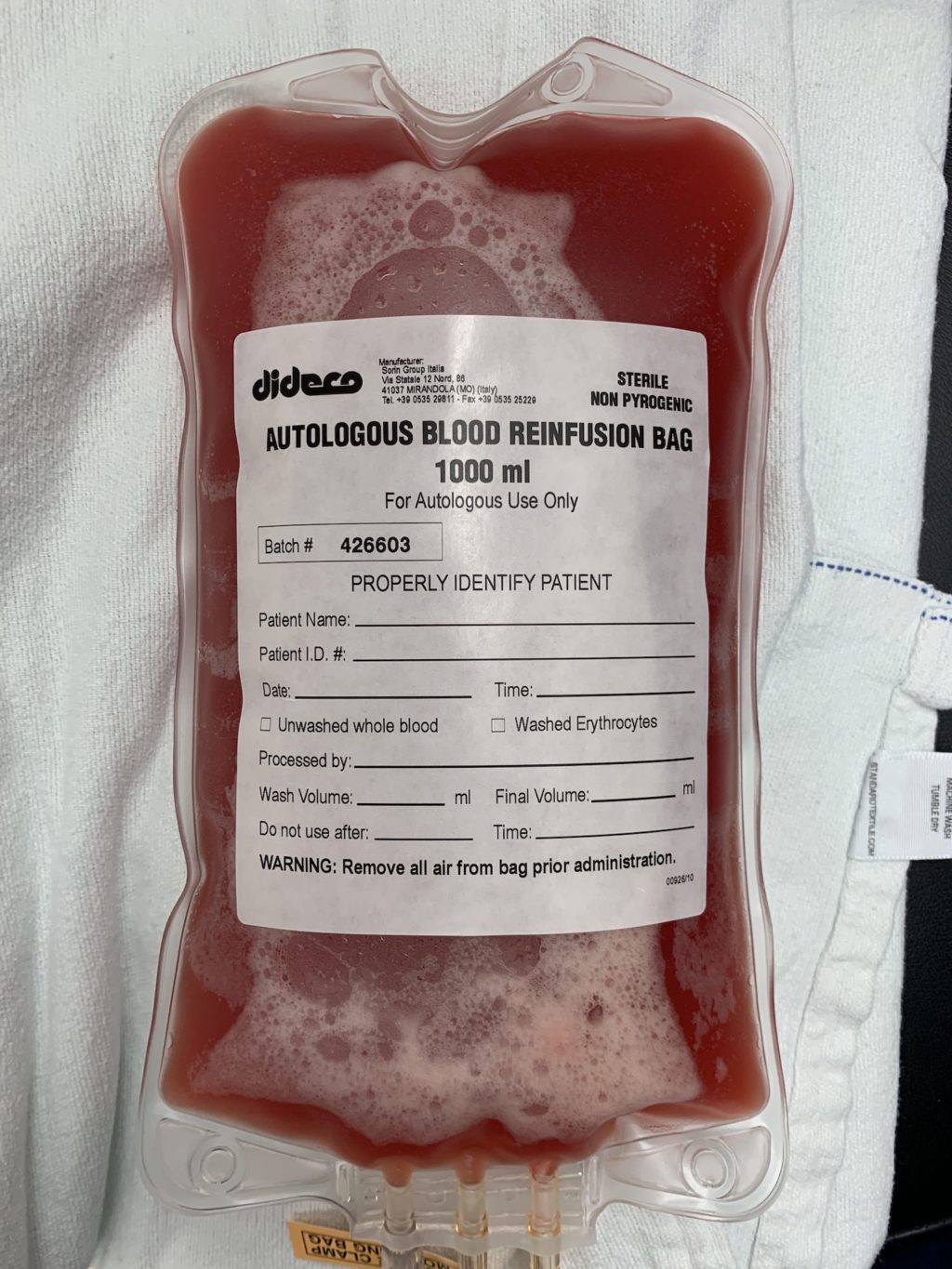
The concept behind IAD is simple: drain whole blood from the patient prior to surgery and reinfuse crystalloid to maintain intravascular volume. In a sense, this “dilutes out” a patient’s blood volume, so when they lose blood during surgery, they are losing less red blood cells per unit volume of fluid lost (acute normovolemic hemodilution). In patients with normal hematocrits, I’ll drain up to a liter of whole blood via a central line into a bag with citrate to prevent coagulation. At that point, my perfusionist colleagues work their magic by spinning down the whole blood into Cell Saver (packed RBCs) and platelet rich plasma (PRP).
Cell Saver can be used on CPB or after coming off bypass as fluid resuscitation in the form of the patient’s own red blood cells. Additionally, since platelet dysfunction is universally expected after cardiopulmonary bypass with hypothermic arrest, I’ll reinfuse the PRP post bypass as well.
Drop me a comment below with questions! 🙂






Why do you have it separated into cell saver and PRP? Why not reinfuse it as whole blood?
Great question! The Cell Saver portion is used for volume while on bypass. The goal is to give the PRP after protamine and surgical hemostasis.