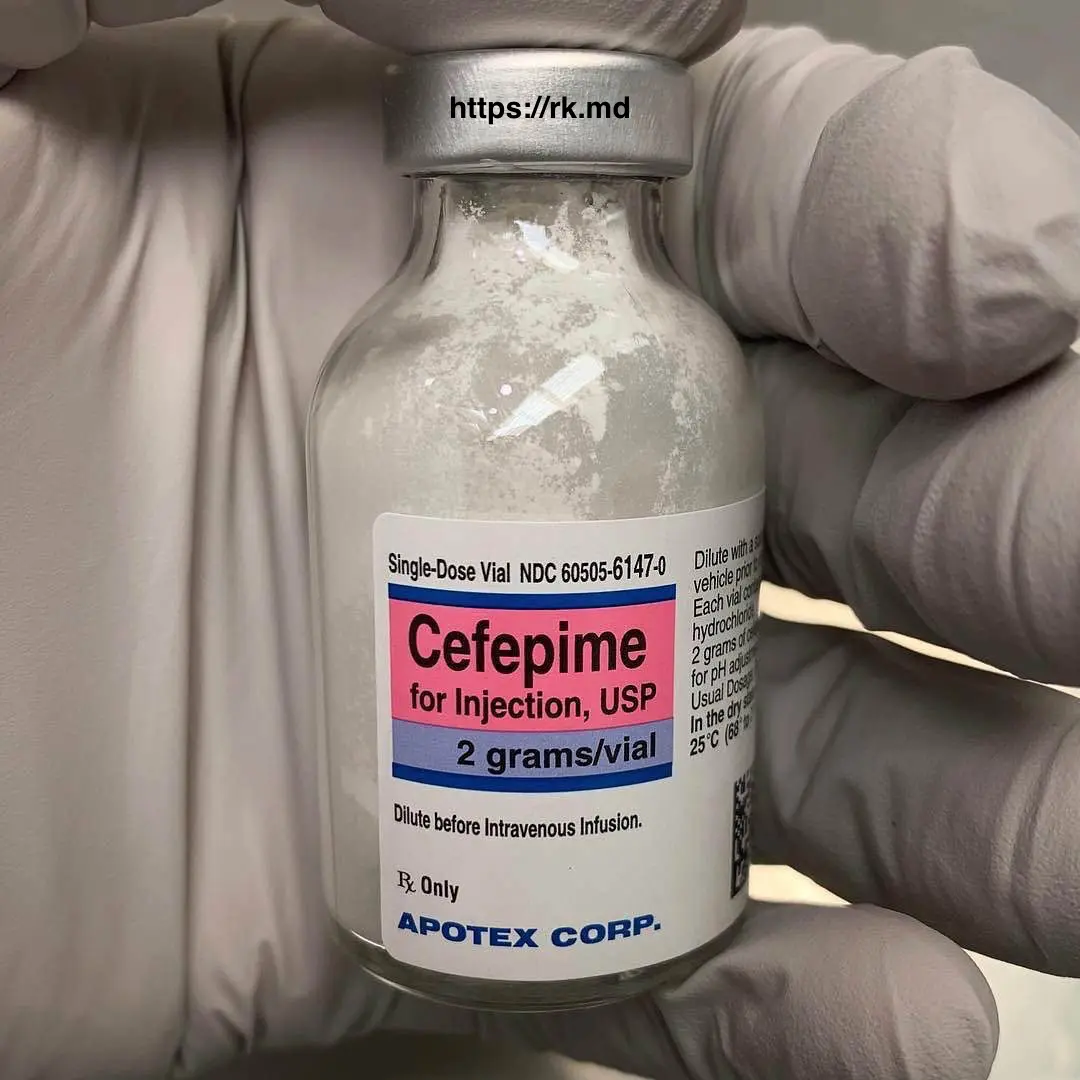
Cefepime (Maxipime) is a broad-spectrum intravenous antibiotic commonly used to treat infections in inpatient and intensive care settings. Cefepime exerts its antibacterial effect by inhibiting bacterial cell wall synthesis. Specifically, it binds to penicillin-binding proteins (PBPs), essential for cell wall synthesis’s final stages. This results in the inhibition of bacterial cell wall synthesis and ultimately leads to bacterial death.
As a fourth-generation cephalosporin, cefepime covers many gram-positive and gram-negative organisms, including Pseudomonas. As an intensivist, I use this antibiotic for everything from hospital-acquired pneumonia to empiric coverage for neutropenic fever and sepsis.
Encephalopathy related to cefepime is a diagnosis of exclusion that can be confounded by the clinical situation itself (e.g., sepsis can certainly cause altered mentation). Nevertheless, it’s important to narrow a patient’s antibiotic regimen when appropriate (antibiotic stewardship!) and always consider the side effects of these powerful medications!
Remember that cefepime does NOT cover methicillin-resistant Staphylococcus aureus (MRSA), Enterococci, and anaerobic organisms. I often combine it with vancomycin and/or metronidazole for MRSA and anaerobic coverage, respectively.