Phentolamine (Regitine) is a reversible α-1 and α-2 blocker used primarily for its vasodilatory effects. When used to control hypertension, one must consider the autonomic effects of blocking these receptors.
Profound vasodilation will lead to hypotension which, in turn, will stimulate baroreceptors (e.g., carotid sinus) to decrease vagal (parasympathetic) and increase sympathetic tone on the heart via norepinephrine release. Norepinephrine’s β-1 effects will increase heart rate (chronotropy) and contractility (inotropy), but because phentolamine also blocks α-2 receptors (normally involved in regulating the release of norepinephrine at the synaptic cleft), the negative feedback loop is lost and potentially even more norepinephrine may be released causing an exaggerated effect of the aforementioned hemodynamic changes (e.g., even more tachycardia). For these reasons, I can’t remember the last time I used phentolamine to control blood pressure.
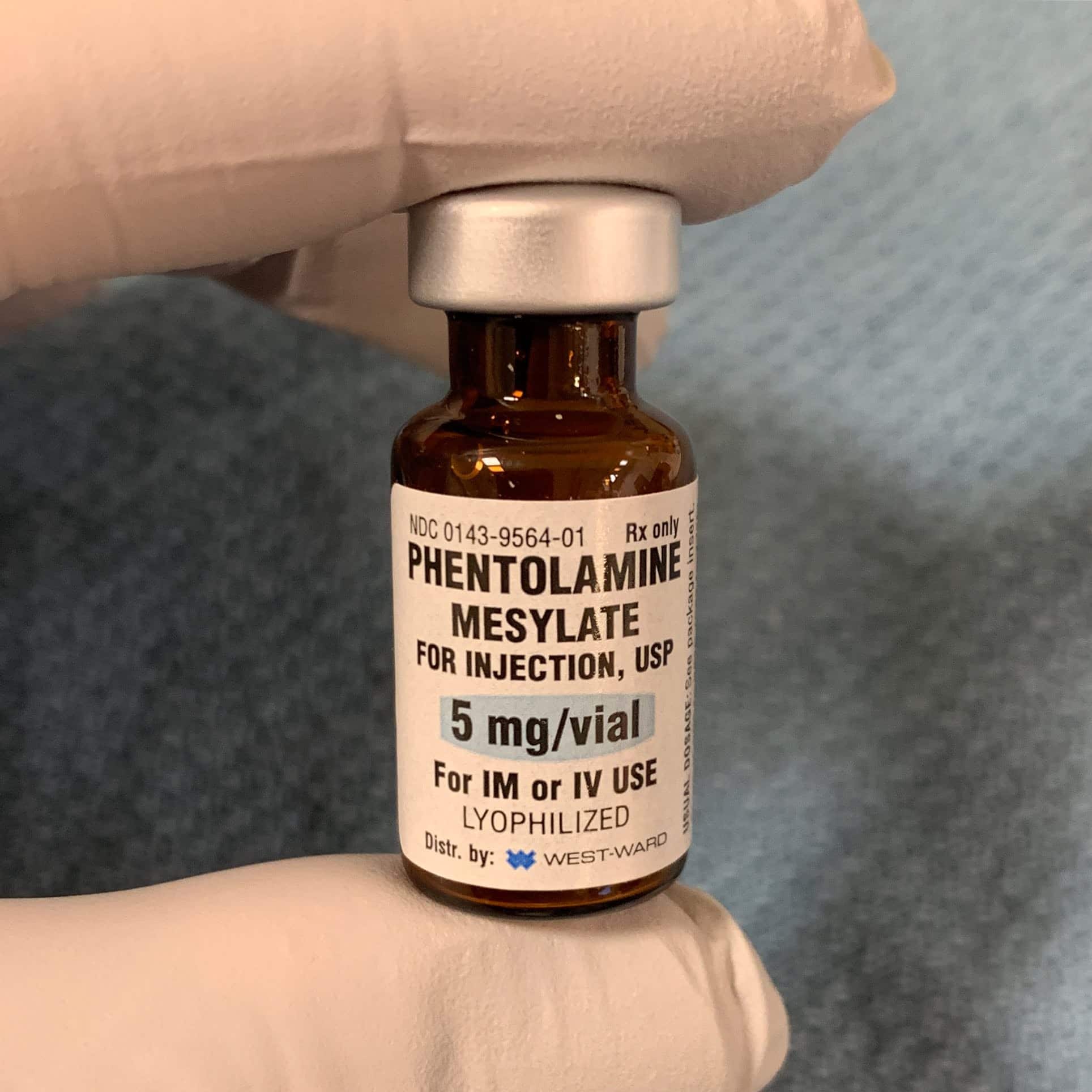
As an intensivist and cardiac anesthesiologist, I’ve seen phentolamine administered as subcutaneous injections surrounding the site of norepinephrine or epinephrine extravasation into soft tissues from a peripheral intravenous line (a rare event, I’ve only seen this once). The idea is that phentolamine will offset the vasoconstrictive effects of pressors to prevent localized tissue necrosis. I infiltrate 10-15 cc of saline containing 5 – 10 mg of phentolamine with a hypodermic needle into the site of pressor extravasation (usually cold and pallid). Immediate redness is a sign of successful sympathetic blockade.
Drop me a comment below with questions! 🙂