Epidural blood patches (EBP) are procedures used to treat post dural puncture headaches (PDPH) refractory to conservative therapies such as NSAIDs, caffeine, hydration, and steroids. As a cardiothoracic anesthesiologist, the most common time I’ll be called to perform an EBP is after a lumbar drain is placed to facilitate cerebrospinal removal for thoracoabdominal aneurysm repairs, proximal thoracic endovascular aorta repairs with debranching, etc. It’s no surprise that a 14 gauge intentional hole into the subarachnoid space can create a CSF leak that isn’t amenable to conventional analgesics. Remember, a lumbar drain is NOT the same thing as a “labor epidural.”
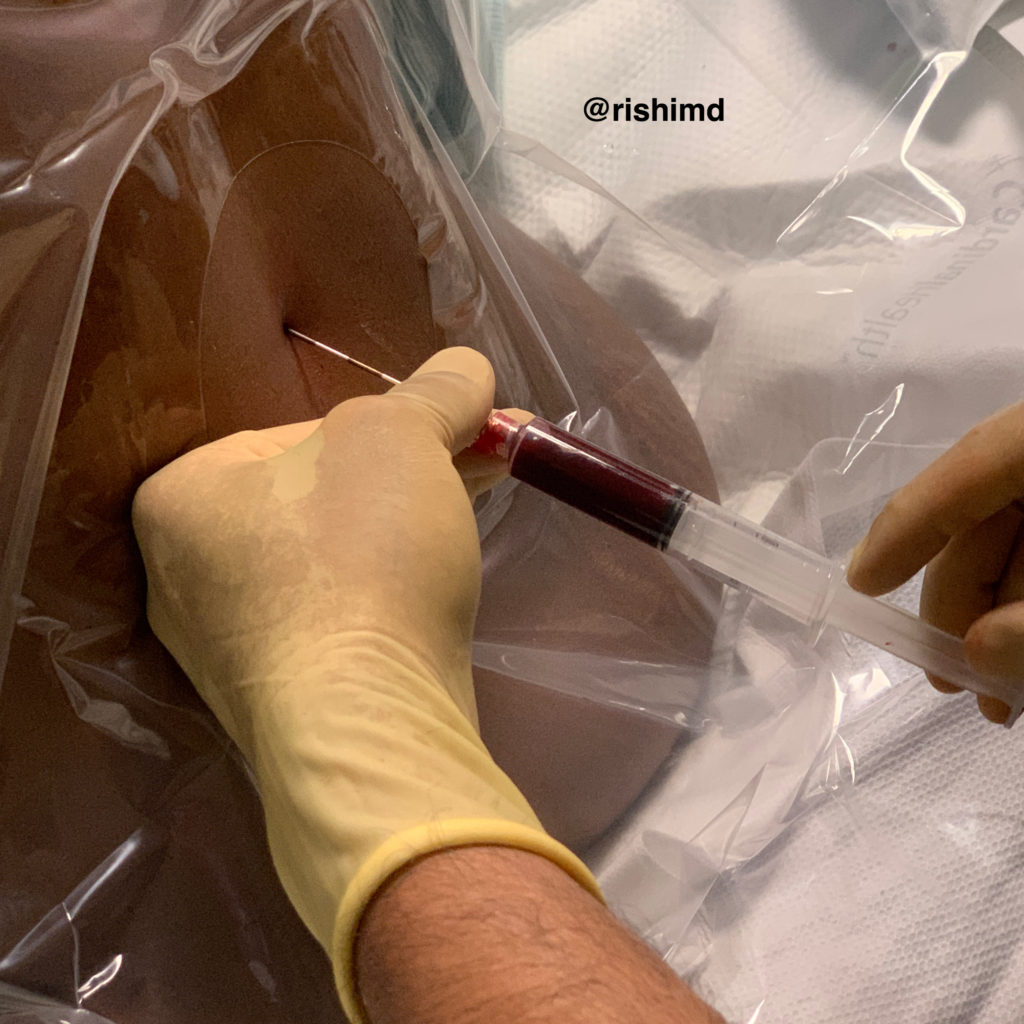
I’ll start the EBP procedure by cleaning my patients back and arm in a sterile fashion. While the prep solution dries, I’ll open my epidural kit. Then, I’ll draw ~20 cc of blood in a syringe and place it on my epidural tray. Next, I’ll access the epidural space in the usual fashion, and proceed to slowly inject blood until the patient feels a sense of pressure. At that point, I’ll remove the Tuohy needle – the procedure is finished!
Before starting an EBP, I’ll double check that my patient doesn’t have any contraindications to neuraxial instrumentation (namely localized infections or coagulopathy). Second, because it’s an invasive procedure… pain, infection and bleeding are all possibilities (although I use plenty of local anesthetic). Finally, although EBP has a very high success rate, there’s always the possibility of creating an inadvertent dural puncture (“wet tap”) as with any epidural.
Drop me a comment below with questions!