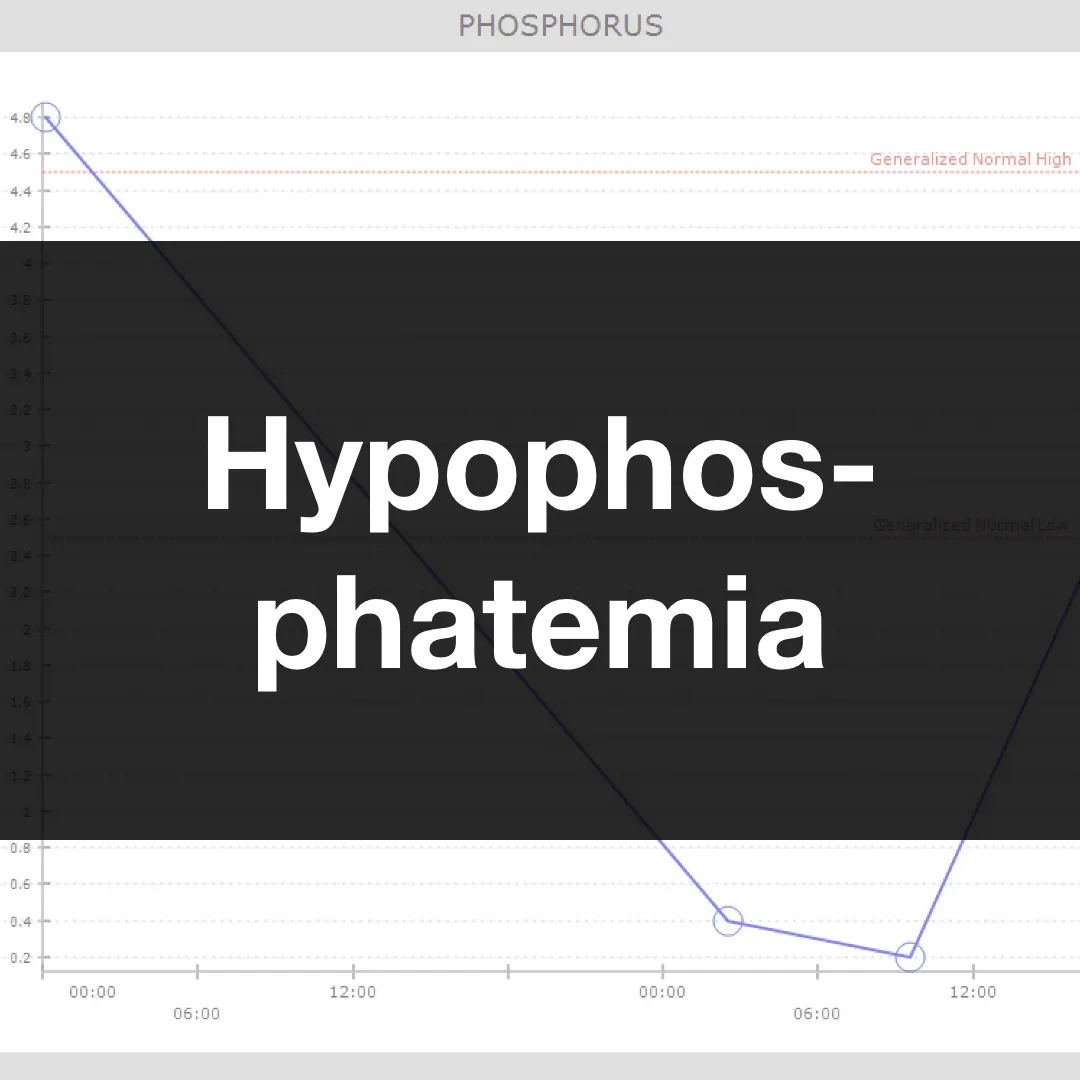
Phosphate is crucial for cellular/energy metabolism, bone integrity, and various enzymatic processes. Hypophosphatemia is classified as mild (2.5-3 mg/dL), moderate (1-2.5 mg/dL), or severe (<1 mg/dL, up to 30% all-cause mortality!) based on serum concentration.
Mechanisms of hypophosphatemia include transcellular shifting (refeeding syndrome, insulin administration, alkalosis), renal losses (primary hyperparathyroidism, diuretics, Fanconi syndrome, proximal tubular dysfunction), poor GI absorption (malnutrition, certain antacids, vitamin D deficiency, NG tube suctioning/vomiting), and extreme catabolism (trauma, sepsis, burns). In particular, patients in diabetic ketoacidosis may have normal plasma phosphate levels (transcellular shifting with acidemia); however, total body stores are often depleted through osmotic diuresis with plasma levels dropping once insulin therapy is initiated.
Remember, the ‘P’ in ‘ATP’ (the body’s energy currency) is phosphate! It follows that symptoms of hypophosphatemia can range from skeletal muscle weakness and rhabdomyolysis to decreased cardiac and diaphragmatic contractility, making it difficult to wean patients from mechanical ventilation. Because phosphate is also an important buffer, the anion gap (AG) used to estimate unmeasured anions is typically lower for patients with low, measurable anions like phosphate and albumin. In other words, if a “normal” AG is ~12 mEq/L, I expect a value lower than that in hypophosphatemia. If a patient is severely hypophosphatemic and has an AG of 12 mEq/L, this suggests the presence of unmeasured anions.