I’m coming off a ridiculously busy Friday call shift, but I wanted to reflect on my first month of being a second year resident (PGY2, or CA1 in anesthesia land). I’ll be honest – at first, I missed aspects of internal medicine. The concept of “working up” a patient is something I thoroughly enjoy (especially when it involved teaching students). Now I’m trying to master technically difficult procedures, pharmacology, and advanced pathophysiology. The anesthesiology learning curve was incredibly steep, but little by little, I’m becoming more comfortable with the nuances of running an anesthetic from start-to-finish. Over the last month, anesthesia has really started to grow on me.
As an intern, many of my upper-level residents and attendings commented that I should consider changing my career to internal medicine as my bedside manner would be “wasted” in anesthesia. The last month proved otherwise. I feel like I’ve really been able to put patients at ease before their operations while providing safe, minimally painful peri-operative procedures. Plus a little Versed helps. 😉
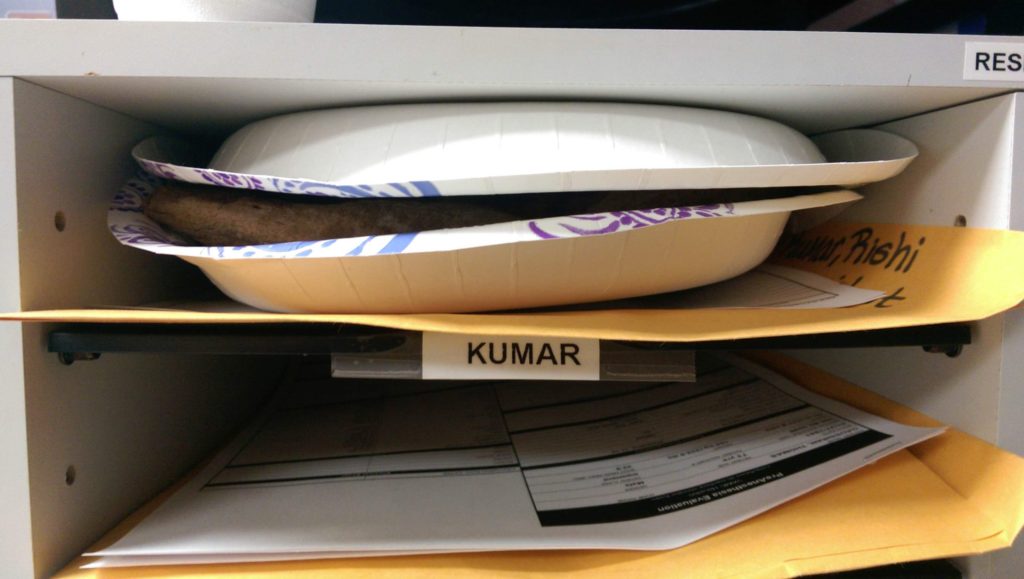
My anesthesia attendings were all wonderful and very “hands-off” too! There are countless recipes to perform an anesthetic, and they empowered me to always find my own style as long as I could justify its utility and safety. This freedom was only facilitated by a great crew of anesthesia techs and equipment. The VA has some incredible airway gadgets (King Vision) and medications (Precedex) which I used throughout the month.
One of the prominent attendings in our program brought up a good point. We often make anesthesia look easy, but there are so many considerations which go into each procedure and anesthetic we employ. A patient’s blood pressure isn’t something we control with a dial on a monitor. Hypercarbia, hypoxemia, and increased peak pressures require explanations. Tachycardia is not always from pain. It takes a great deal of integrating pathophysiology with pharmacology to safely practice in this field.
The VA patients are older with the extremes of disease pathologies – severe congestive heart failure, end-stage liver disease, end-stage renal disease, vasculopaths, hepatitis/HIV, metastatic cancer, and the like. Learning to safely perform anesthesia in these patients in my first month was nerve-wrenching at first, but in retrospect I’m better for it. I’ve done countless peripheral, arterial, and central lines as well as difficult airway intubations. My cases ranged from open heart surgery and 10 hour vascular cases to simple trigger finger releases. By sheer volume, I’m learning the special considerations to have for a given surgical case.
Now that I’m back at our level 1 trauma center this month, I’ll once again be thrown into a new environment. The machines are different. The medication carts are different. Trauma will be entirely new. The attendings are new. 😯







Hey Rishi, I’m in my internal medicine prelim year right now. I’m really worried about starting CA-1 year behind everyone else as I don’t have any anesthesia rotations, just about 3.5 months of MICU is about as close as it gets. Any tips for me or things to allay my fears? I do plan on reading M&M through by the start of CA-1. Thanks
This is a common fear for prelims! Having seen multiple classes of prelims join the categorical residents each year, you will be FINE with regards to your knowledge base and in-training exams. You’re already taking great initiative by studying M&M, so keep up the great work! Don’t be frustrated that a lot of anesthesiology might be over your head at this point. Focus on things you can learn – medications (doses, side effects, etc.), physiology, relevant equations, etc. I promise the rest will come to you once you start as a CA-1!