It’s fairly rare for anesthesia residents to pursue a dual fellowship, but for those who do, the combination of critical care and adult cardiothoracic anesthesiology is common. After being asked by family members and friends why I want to extend my training by another two years, I decided to outline the reasons which led me to this decision.
SPECTACLE OF RECOVERY
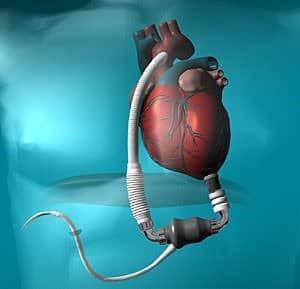
Mechanical ventilation, continuous renal-replacement therapy, vasopressors, extracorporeal membranous oxygenation (ECMO), a plethora of invasive monitors, and the like are all commonplace as one walks through the intensive care unit (ICU). While many ICU patients face terminal diagnoses and even more are successfully transferred out of the unit to deal with chronic comorbidities… a small sample experiences something more profound. Individuals who should not have survived – those that were an inch from death and on every support device imaginable who turn around and literally walk out of the hospital weeks-to-months later. It makes me redefine what actually constitutes a “terminal diagnosis” and gives me hope that with the right interventions (usually requiring ICU care), anyone is subject to improve no matter how unlikely.
KNOWLEDGE
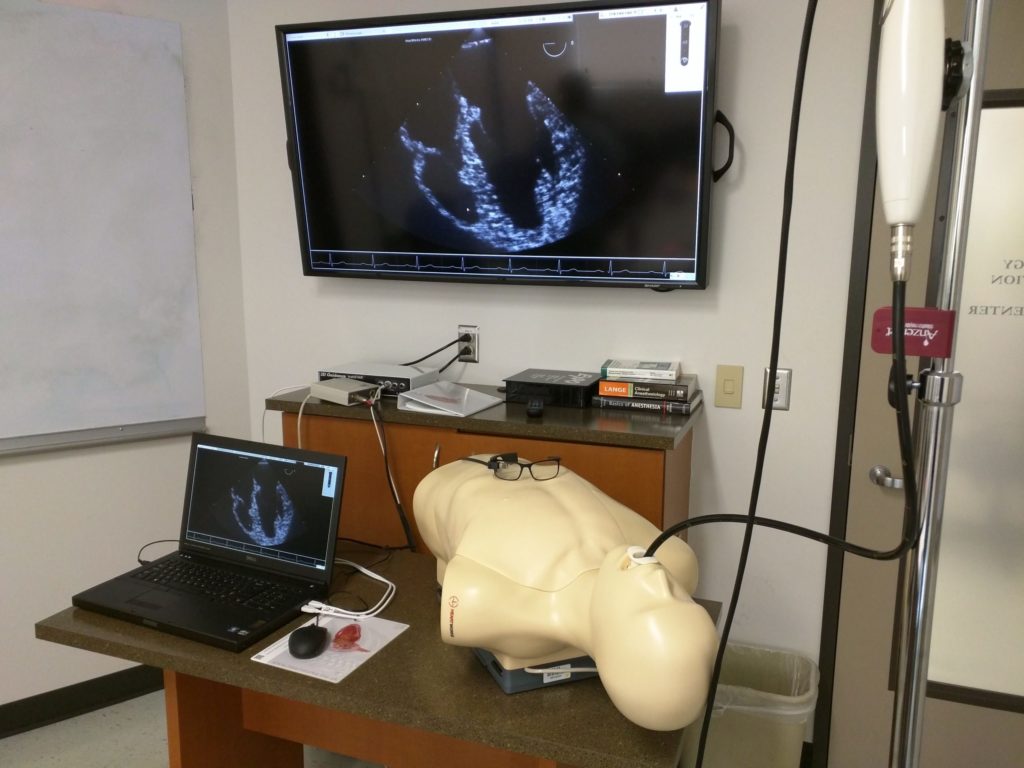
I’ve witnessed how fragile patients with severe cardiovascular comorbidities can be in the perioperative setting. Relatively new to anesthesiology, I initially drew on my ICU base to care for these patients, but found myself with large knowledge gaps in echocardiography, intracardiac devices, and cardiopulmonary bypass. I then realized how a dual fellowship in critical care and adult cardiothoracic anesthesiology will empower me with the skills to become a more complete perioperative physician – one who not only understands the complex pathophysiology of life threatening ailments but is also skilled to appropriately diagnose and intervene in the operating room or ICU.
CONSULTANT
It’s disheartening how often consulting services ridicule the primary team. We know you’re busy. We know you have a finite amount of time to see a growing number of patients. The fact that a consult is placed already means the primary team needed help from a team or individual with more expertise. There’s no need to belittle or seek validation for your efforts.
My mentors have taught me that true power comes from being so in tune with one’s abilities that one no longer thrives off of recognition but off of knowing the right thing was done for the patient. I want to be the friendly consultant intensivist colleagues turn to for answers.
CHALLENGE
Throughout my residency training in anesthesiology, I’ve developed a desire to accept the most challenging cases. Rather than shying away from complexity, I have grown substantially by working alongside our intensivists and trauma/cardiothoracic anesthesiologists to polish my mindset and procedural skills during our patients’ most desperate hours. Prioritizing the steps in resuscitation and learning to communicate with all the involved treatment teams are pivotal characteristics of a perioperative physician which often translate to safer and better outcomes.
These two fellowships will be extremely challenging. The hours are difficult. All the patients have severe, acute issues. Often times, even the social aspect of end-of-life care trumps the medicine itself. I find these challenges appealing. 😀
TRAINING AND CAREER GOALS
I now seek rigorous training in both fellowships to expand my breadth of diagnostics, familiarity with treatment modalities, procedural finesse, and ability to rapidly apply my full array of skills to help in any clinical situation. Starting with critical care will provide an unparalleled foundation in pathophysiology to build upon as a cardiothoracic anesthesiologist.
I want to continue practicing how to effectively establish rapport, alleviate anxiety, and distill complex medical pathophysiology into simple concepts. These traits will combine with a sincere empathy to help many patients and their families deal with end of life care – a reality for many critically ill patients.
The synergy of my medical knowledge and technical skills coupled with a strong work ethic and laidback persona make me well-fitted for a career as a perioperative academician. One day I hope to work alongside medical students, residents, and fellows to teach and mentor the next generation of perioperative physicians.
LIFE CIRCUMSTANCES
Although it’ll likely be the first time I leave Houston for education or training, it’s time to learn how medicine is practiced elsewhere! I can bring these techniques back to the Texas Medical Center or wherever I end up working.
It’s not practical for me to finish residency, work, and then come back for fellowship. This is my chance to finish all of my training in one shot and then settle down as far as a career, marriage, etc. 😯
…and this is why I’m pursuing a dual fellowship in critical care and cardiothoracic anesthesiology.
The San Francisco Match opened for critical care anesthesiology on November 2nd, and I submitted my application materials by November 8th. Just waiting for all my recommendation letters to find their way to the programs. Hope the interview trail is nice to me. 🙂






Hi,
I am a CA-2 that applied to dual fellowship – Critical and CT. I have interviews coming. Any advice?
Given that interviews are virtual which limits things for both the program and interviewee, best advice is to be oneself. Most programs have already reviewed/screened applicants – you just want to see if you feel like you’re a “good fit” based on people you interact with, the city the program is in, etc.
Hi Rishi,
I’m currently on ICU elective and enjoying it and am planning on applying to Anesthesiology for residency this year.
Are there any Anesthesiology-CCM jobs in private practice where you can work 50/50 OR:ICU or say 3 weeks of a month in OR 1 week ICU? The only such combinations I hear and from my own personal job search is in the Academic setting. Thank you for your time.
Hey Paul! To be honest, I don’t know any anesthesia-trained intensivists outside of academics. They have varying amounts of ICU time relative to OR time. For me, I’ll ultimately be 50-50 between cardiothoracic anesthesia and critical care.
Hey Rishi,
Thanks for your response. I’ve thought about what you’ve said for the past week while working in ICU elective and have more questions.
There are a few combined 5 year Anesthesiology-Internal Medicine residency programs such as at Stanford, UC Irvine, Loma Linda in Cali, Medical College of Wisconsin etc and most of the graduates of those combined residencies pursue critical care fellowship via Anesthesiology route afterwards(they do IM as well due to gaining a “more established knowledge base and expertise” in medicine overall that will give them upper edge in CCM). With that said, do you feel the 1 Year CCM fellowship vía the Anesthesiology route is at anyway deficient vs a IM-Pulmonary/CCM pathway as an intensivist? I.e. do you feel less competent than your pulm/crib colleagues in the ICU?
I ask because I don’t see a point in doing the 5 year combined with Internal Medicine IF a person will be just as competent and knowledgeable being an Intensivist via the Anesthesiology route. As a result, would you recommend doing the five year combined residency?
How you answer will play a significant role in whether I apply to the combined 5 year or not next month for the Match. Thank you for your time.
I feel extremely competent in the ICU arena. The reality is that from anesthesia training alone, you become comfortable with many “ICU” things: ventilator management, procedures, titrating medications to achieve hemodynamic goals, etc. Sure, an internal medicine background coupled with a pulmonary fellowship will certainly stand on its own in terms of the breadth of knowledge regarding chronic conditions (COPD, OSA, ILD, etc.), but in the acute setting, I did not feel less competent at ALL.
Needless to say, this is also very dependent on the individual. I immersed myself in the literature/text to gain a deeper understanding of this field, and in doing so, developed a broader appreciation of pathophysiology, pharmacology, and evidence-based practice. If you’re lazy, you may indeed feel deficient. Hope this helps!
Hi Rishi,
Thank you for always responding to my questions.
Which textbook did you primarily use to learn during anesthesiology residency? Basics of Anesthesia by Miller or Morgan and Mikhails Clinical Anesthesia or some other text? I checked your textbook tab but you listed many of the textbooks out there in the field of anesthesia in general so I don’t know which one you used primarily.
Does anyone still use Big Miller in residency? The 9th edition is coming in a couple months. Would you recommend investing in that or is it unnecessary for Anesthesiology residency?
I DEFINITELY used Big Miller (8th edition) during the course of my residency. Our didactics were out of Barash, but I think either of these textbooks is important for physicians to read. Yes, it’s a long book, but I always preferred having one source over many. Morgan & Mikhail is too basic of a text.
Hi Rishi.
At what stage of your medical career did you realize you wanted to enter:
1. Anesthesiology
2. Pursue dual fellowship in CTA/CCM
-which point did you know that you wanted to stay in academics vs private practice?
On that note: don’t you want to do your own cases in the OR as an attending instead of letting the residents run the cases? I mean, sure you are present at induction and emergence, but didn’t the typical anesthesiologist choose anesthesia because THEY wanted to do the procedures>put ivs in, intubate, draw meds, administer meds, instead of letting someone else do it. I mean sure, we have anesthesia care model of anesthesiologists supervising AAs or CRNAs in certain practice settings but still…
3. If you had gone into private practice instead of academics, would you still have pursued two fellowships of CT anesthesia and CCM or just CT anesthesia?
Thank you for your responses.
Hey Paul!
1.) Didn’t shift to anesthesia till the end of my third year of med school. I thought I was going to be doing neurosurgery until then, but fell in love with the unique aspects of anesthesia (administering my own meds, the OR environment, needing to understand global pathophysiology/pharmacology over a single organ system, hemodynamic/airway management, and lots of procedures).
2.) I also fell in love with taking care of critically ill patients in the ICU as well as modalities like 3D TEE and mechanical circulatory support in the cardiac operating rooms. There’s a lot of synergy between the two fellowships, and I feel that being an intensivist makes me a better cardiothoracic anesthesiologist (and vice versa). I don’t understand the (common) misconception that people in academics don’t do their own cases. I do plenty of them (even moonlighting additional days doing my own cases). Also, I’m not just “present at induction and emergence.” Being a good academician is (in my opinion), a fine balance between flexibility, autonomy, and being a good educator. I’m a huge proponent for intraoperative teaching tailored for the case at hand, reviewing hypothetical scenarios, board review, etc. There’s really only one area where I’m truly in a supervisory role with my AA colleagues, but that’s probably 10% of my job (even less if you consider my intensivist role).
3.) I did two fellowships for my OWN edification, not to land a particular job. I wanted to be the best trained perioperative physician I could be which extends way beyond being able to intubate and turn on a vaporizer. This is a message I try to drive home with my residents/fellows – they are physicians first, and then anesthesiologists. I push them to read, do research, be stewards of patient safety, and rely on their unique training as decision makers to make difficult calls.
Thanks for writing this up. Current fourth year medical student reading up on as much about anesthesiology as I can and posts like this help!!!
You’re very welcome! 🙂
Great post, dude! 🙂 Are there many of these dual fellowships around? Or do you have to apply, first, to like CC, finish that, then apply for CT? Just wondering how it works. I’m not there yet (still just a mere med student, though non-trad), but it sounds so awesome the way you put it! 🙂
Thanks Pat! So there are a few unofficial “combined” fellowships, but the majority of applicants have to apply to each fellowship separately and match twice. Cumbersome process… but I think it’s worth it! 🙂