Maintaining coronary perfusion pressure (CPP) is arguably the most important objective in cardiac anesthesiology. CPP is defined as the difference between aortic diastolic pressure (AoDP) and left ventricular end-diastolic pressure (LVEDP) when describing perfusion to the left ventricle.
CPP = AoDP – LVEDP
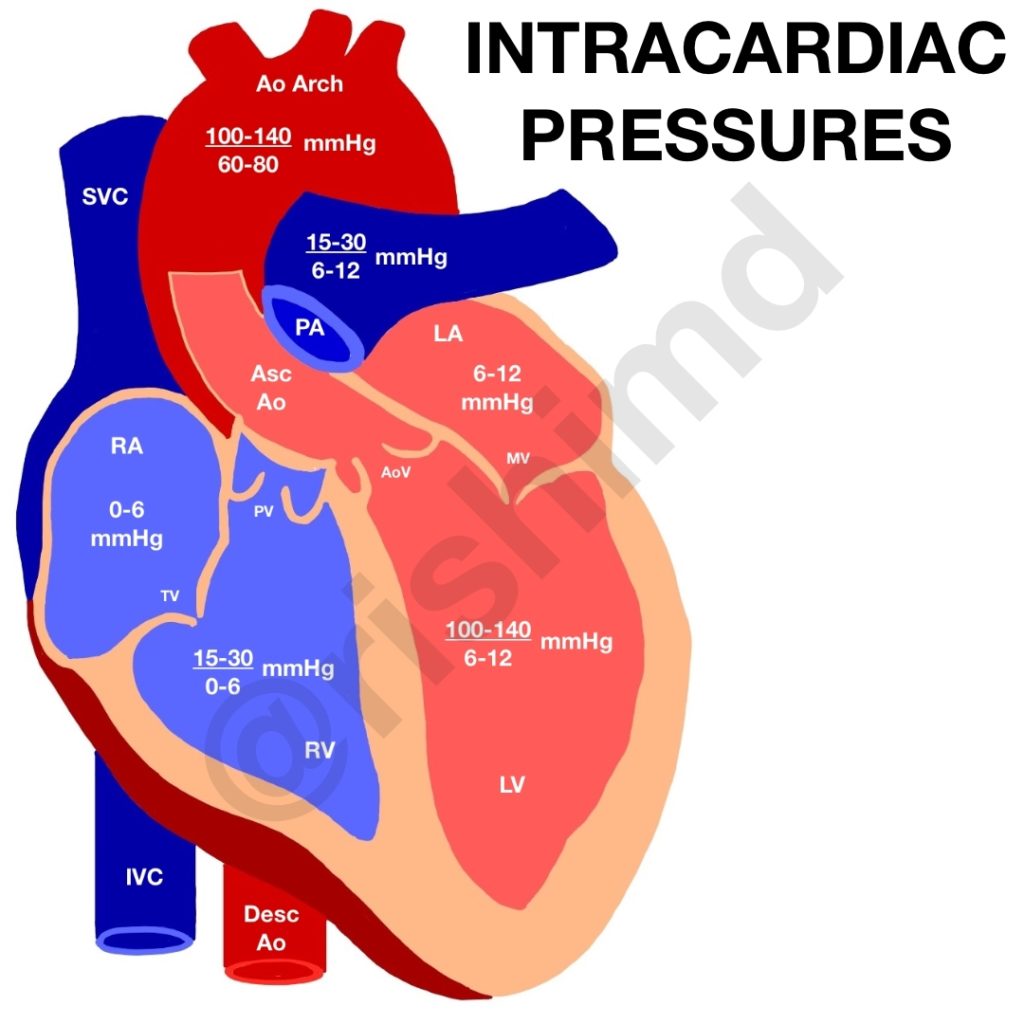
Coronary arteries originate from the aortic root, so aortic pressures (Ao) relative to right ventricle (RV) and left ventricle (LV) pressures create gradients driving blood flow down the coronaries. For example, let’s look at the aorto-ventricular gradient on the right ventricle during systole and diastole:
Δ(P)systolic = Aosystolic – RVsystolic = 140 – 30 = +110
Δ(P)diastolic = Aodiastolic – RVdiastolic = 80 – 6 = +74
The positive gradients explain why the RV is perfused during both systole and diastole. Now let’s do the same calculation for the left side.
Δ(P)systolic = Aosystolic – LVsystolic = 140 – 140 = 0
Δ(P)diastolic = Aodiastolic – LVdiastolic = 80 – 12 = +68
The LV is only perfused during diastole because there is little to no gradient during systole (zero in the above calculation).
Here’s a practical application. Let’s say you’re coming off cardiopulmonary bypass, the patient is hypotensive, and the heart has very poor contractility on transesophageal echocardiography. You have two choices – give a pure inotrope to improve contractility or a pure afterload enhancer to increase blood pressure.
A pure inotrope will only increase myocardial oxygen demand, but an afterload enhancer (like norepinephrine or vasopressin) will increase both myocardial oxygen supply (by increasing the CPP) as well as the demand (due to increased afterload). This increased coronary perfusion is vital to reperfuse the myocardium adequately.
This concept is also why we give such high doses of epinephrine and vasopressin during ACLS resuscitations. The epinephrine isn’t intended to “jump start” the heart directly. Instead, it causes massive vasoconstriction to (hopefully) increase coronary perfusion and restore myocardial function.