It’s important for the intensive care unit (ICU) treatment team to construct and communicate our daily assessment and plan with all relevant parties involved in a patient’s care. We accomplish this during “rounds” each morning with a team usually led by the ICU fellow consisting of the patient’s nurse, an attending physician, residents/PAs, medical students, and clinical pharmacists/students. We’ll also have dieticians, respiratory therapists, consultants, speech and language pathologists, physical therapy, occupational therapy, and care coordinators often provide recommendations during rounds.
As a critical care fellow, my job is to oversee the education of trainees, maximize workflow efficiency, and most importantly promote the care and safety of our patients. On a normal day shift in our combined surgical, burn, and trauma ICU, I usually receive handoff from the overnight fellow around 6:45 AM and proceed to the unit by 7:00 AM. By this point, the daytime residents/PAs have also received handoff from the overnight resident and are busy working on dividing the patient census, reviewing overnight events, gathering data, and working on progress notes before rounds start at 7:45 AM. I’ll check and make sure they don’t have any immediate issues or concerns before proceeding to walk around the unit on my own starting with the most critical patients.
I have a sequence of steps I always perform, no matter how sick the patient, to ensure I don’t miss anything important before rounds.
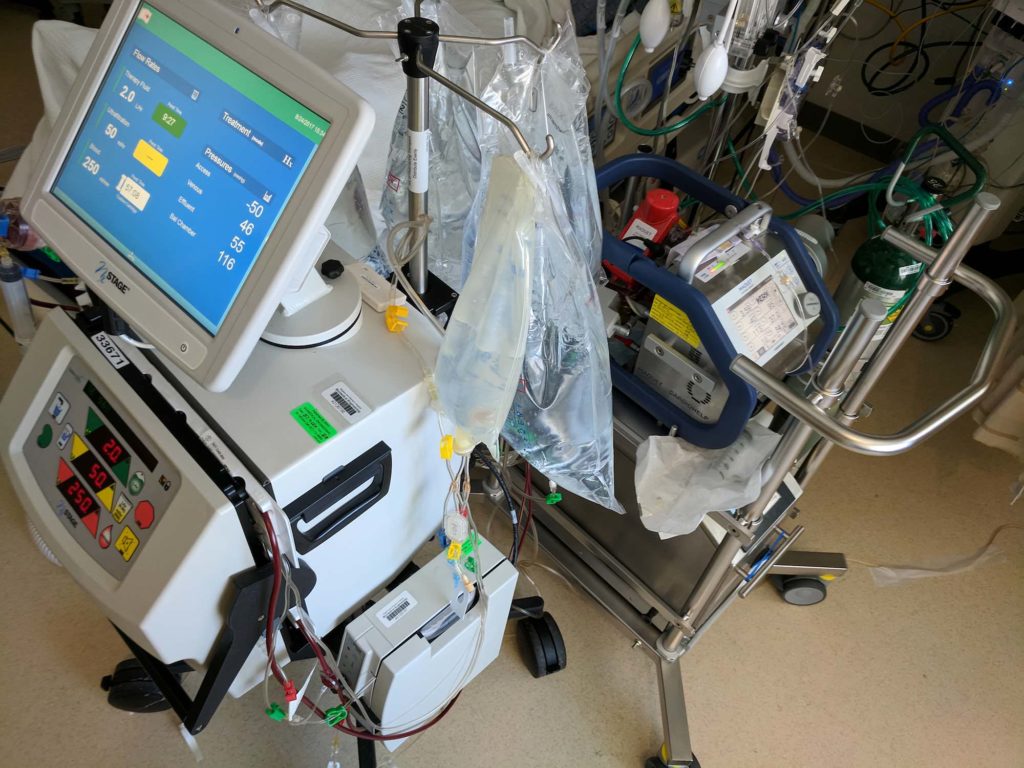
- Look at every patient. This doesn’t necessarily mean do a full exam, but at least laying eyes on every patient is critical as one can gather so much information. Are they delirious? Are they sleeping? Are they awake in a chair? Are they in pain?
- Talk to the nurses about overnight issues, concerns, and if the treatment plan seems reasonable thus far.
- Review the current vital signs, urine/drain output, telemetry data, and imaging
- Perform focused physical exams (including bedside ultrasound) when appropriate
- Discuss ventilator management and weaning with the respiratory therapist
- Discuss potential transfers and admissions with the charge nurse
- Review orders. Notes are important for billing and communication across disciplines, but it’s the orders which guide patient care.
Doing all of this for a full census usually takes less than 30 minutes, but it gives me a general idea which patients are improving, which are stable, and which are deteriorating. The details are then discussed on rounds with the full team.






I am a fellow right now. Never quite sure about what/how to contribute during rounds esp since i am anesthesia-trained like you. Any other advice?
It doesn’t matter if you’re anesthesia-trained, surgery-trained, internal med trained, or EM-trained – I think it’s important to study the relevant pathophysiology of your patients ahead of time, have a game plan before rounds, and let your voice be heard. Also, listing all the possibilities isn’t helpful. As a fellow, you need to stratify which options are the “best”, and commit to one knowing that you might be wrong. Also, discuss expectations with your attending too.
Amazing. Love the practical advice. It crosses all displines in health care. Yes, collaborative care! Thank you for rebuilding health care from the ground up 🙂
I’m doing my (little) part! 🙂
This is awesome! Very informative. Thanks for sharing…
Thanks so much, La’Tila! 🙂
How do you organize your daily notes or keep track of all your patients as a fellow? Still use the same scut sheets as an intern or do you just remember everything? Haha
We round with portable computers, so if we need to look up specific vitals/labs, we can just look in the electronic health record (EHR). I tend to remember most of the important things (antibiotics, pressors, nutrition, ventilator settings, etc.)