The pulse oximeter (“pulse ox“) is perhaps the best non-invasive, continuous monitor ever created. It uses a light emitter and photodetector to analyze light absorbance across an extremity (typically a finger or toe). In doing so, the pulse ox gives us the hemoglobin oxygen saturation, heart rate, a rough idea of the rhythm, and even the fact that there’s distal perfusion present with the aid of a waveform.
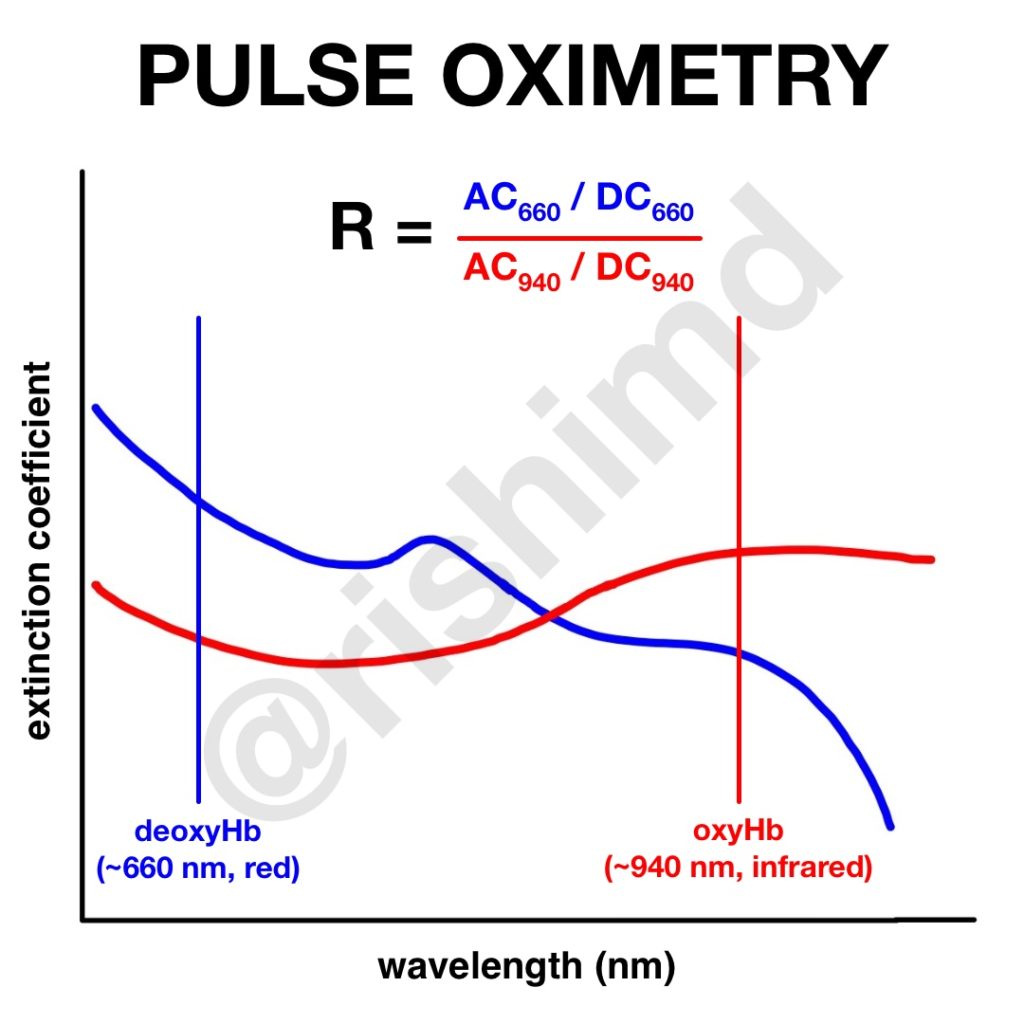
Oxyhemoglobin (oxyHb) and deoxyhemoglobin (deoxyHb) have varying absorbances of light across different wavelengths. The extinction coefficient describes the degree to which oxyHb and deoxyHb absorb light at a given wavelength (940 nm and 660 nm, respectively). These two wavelengths are selected to maximize the ratios of the absorbances. In other words, at 660 nm (red), the deoxyHb to oxyHb ratio is maximized, where at 940 nm (infrared), the converse is true.
The key to an accurate pulse ox reading is minimizing noise and amplifying the arterial signal. The pulse ox picks up an arterial component (‘AC’) and a nonpulsatile component (‘DC’). The ratio (‘R’) of AC to DC at the 660 nm and 940 nm wavelengths is determined. This ratio is then correlated to a hemoglobin oxygen saturation based on a calibration curve derived from desaturation studies in healthy patients. SpO2 is unreliable below ~70% because, well, it’s unethical to have volunteers desaturate below that. Mathematical models try to extrapolate desaturation < 70%.
Drop me a comment below with questions and read my post on what pulse oximeters tell us.






Hello Dr.Rishi
I Liked your topic and it’s so helpful. I really had a lot of questions to ask about this pulse Oximetery topic.Because I always have asthma and COPD pt who have low O2,but it considered normal for them even pt tells me “it’s normal for me”Which we end up giving them nebulizer even if there Oxygen 96-97. Also, I have seen pt who have SOB but if I check thier O2 it’s 95% and I don’t see any color change on them. As well we do see children in our clinic and the parents will tell me that thier child is very sick and fussy all night I check all V/S his/her and it looks normal. Some doc consider an O2 of 96 is bad for child and they order nublizer. They decided that after they have listen to pt lungs and they don’t depend on monitor only. They tell me his/her lungs are not clear. Therefore, he need treatment.
I guess you don’t see perdiartic pt cause on your topic you didn’t mention anything about them and you didn’t mention the ideal O2 for children. I would like to know what is your expectations of asthma,smokers,and COPD pt of O2. Hope didn’t bother you with my questions
Thanks!
For patients with asthma, nebulizers tend to help with airway reactivity which may or may not make a huge difference with oxygenation. It’s important to also consider the ventilation component of respiration (removal of carbon dioxide). In COPD patients, I tend to prefer pulse ox saturations in the low 90s because of the Haldane effect and worsening V/Q mismatch.