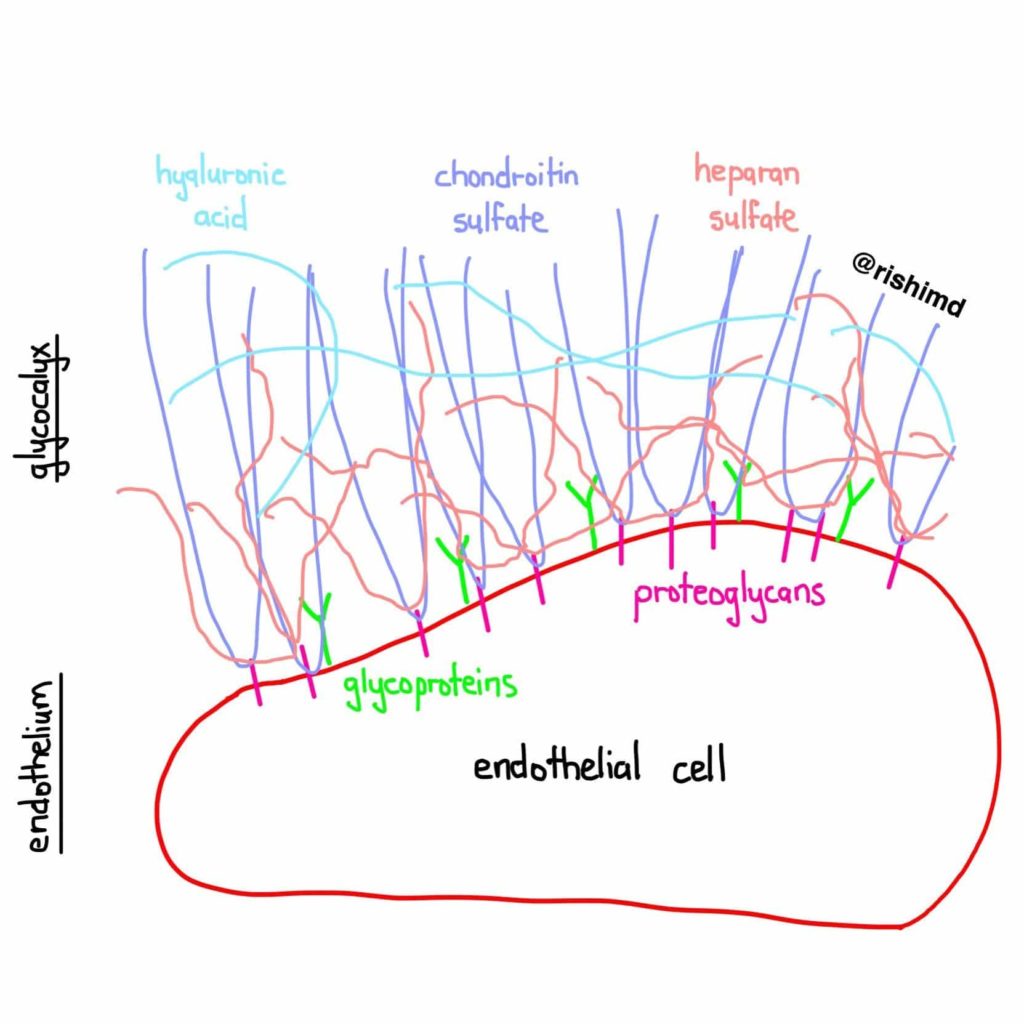
The glycocalyx is a surface layer of proteins lining the luminal (blood-containing) side of vascular endothelium. It plays an important role as a vascular barrier, provides structural support, facilitates cellular interactions, mitigates vasomotor tone, and has a role in the inflammatory and coagulation cascades. Substances like chondroitin sulfate, hyaluronic acid, and heparan sulfate form a scaffold while glycoproteins like syndecan-1 and glypican anchor many of these molecules into the apical membrane to form this incredibly important layer!
In addition to sepsis, mechanical/chemical trauma, hyperglycemia, ischemia-reperfusion, shock, endotoxins and inflammatory states, even crystalloids (which are often used to TREAT illness) disrupt the glycocalyx. In response to the aforementioned states, the glycocalyx is bombarded with degradative enzymes (metalloproteinase, sialidase, heparanase, hyaluronidase, etc.) The resulting collapse can lead to “vascular leak” coupled with vasomotor, hematologic, and immunologic derangements.
There’s a tremendous amount of research investigating how we should go about protecting this layer. Some have suggested a low protein state to promote the degradation of the glycocalyx thereby favoring the use of fluids like albumin and even fresh frozen plasma, the latter of which may also contain restorative proteins. Others are trying to identify exactly which molecular pathways are helpful and harmful to determine how to best swing the balance on favor of glycocalyx protection/repair. We just don’t know!
It’ll be interesting to see where research takes critical care over the next decade… perhaps strong evidence in favor of the EARLY initiation of vasoactives/inotropes rather than fluid loading all patients who hit the ICU?
Drop me a comment with questions below! 🙂






So, what are your thoughts re the results? https://clinicaltrials.gov/study/NCT03434028?tab=results
Hey! Would love to use your glycocalyx pic for my iFAD talk next week, credited, naturally… May I?
thanks!
@ThinkingCC
Hey Phillipe! Feel free to use it! Thanks for letting me know! 🙂
What inotropes and vasoactives specifically are you recommending? Digoxin? ACE receptor blockers? ACE inhibitors? Thanks for a very interesting look at a complex area. It is refreshing to read a research level type article. I was a physiologist before I was a doctor, and so am always looking for physiology behind the medicine. Jill Karatinos MD
Thanks for the comment! I’m honestly not recommending anything in particular, but just suggesting that the notion of needing to “aggressively volume resuscitate BEFORE starting pressors/inotropes” might not entirely be true. One of the big ongoing studies (link here) looking at liberal crystalloid usage vs early vasopressor initiation is using norepinephrine (which makes sense given the evidence for it in pathologies like septic shock).