Pulmonary hypertension (PH) is a broad topic encompassing primary and secondary etiologies. Like systemic hypertension, PH refers to elevated pressures in the pulmonary vessels. It’s essential to understand how PH is classified and which specific vessels are involved: pulmonary arteries → pulmonary capillaries → pulmonary veins.
PRE-capillary PH refers to elevated pulmonary ARTERIAL pressures, and POST-capillary refers to pulmonary VENOUS hypertension. For example, it makes sense that WHO Group 2 PH (caused by left heart issues) will initially increase pulmonary venous pressures as blood flow is directed backward. In reality, many patients with PH have both arterial and venous problems.
Symptoms can initially be relatively nonspecific and include exertion dyspnea and fatigue. As the severity worsens, signs of overt right heart failure may predominate. The history/physical exam combined with echocardiography, labs, EKG, and cardiac catheterization can help hone in on the diagnosis. In addition, the functional classification helps me ascertain the day-to-day limitations a patient’s PH has incurred to help me gauge how “sick” they might be in the ICU or OR when faced with other clinical situations (septic shock, complex cardiac surgeries, etc.)
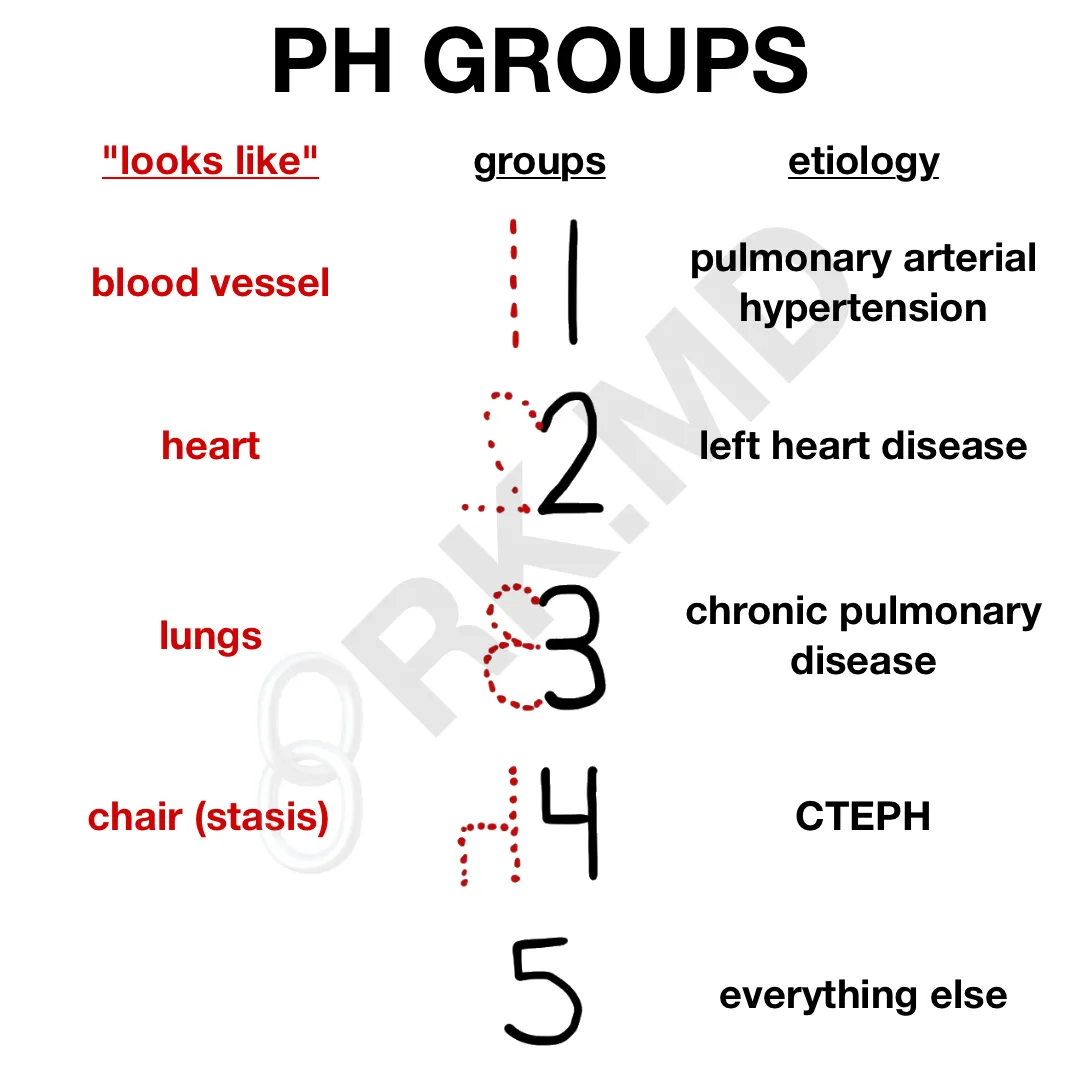
I remember the PH groups by writing the number and looking at its mirror or flipped image. For example, ‘1’ looks like a blood vessel (pulmonary arterial hypertension). ‘2’ mirrored on itself looks like a heart (left heart disease). ‘3’ mirrored on itself resembles a pair of lungs (chronic pulmonary disease). ‘4’ flipped vertically looks like a chair suggestive of stasis and clot formation (CTEPH). ‘5’ is everything else!
Drop me a comment below with questions!







Thank you for the informative post. I just wanted to point out that 2019 WSPH guidelines suggested using mPAP > 20 for diagnosis of pulmonary hypertension vs. 25.
Thanks for the comment! I received several messages regarding the proposed revisions, and although the PVR parameter seemed to be more agreed upon, several pHTN experts reached out to me saying the 20/25 mmHg threshold was still a bit controversial. With that said, I went ahead and updated the table to reflect the proposed definition of mPAP > 20 mmHg.
If you have a patient that comes to OR with pulm HTN, what are some of your recommendations to minimize potentially worsening their condition? Avoid hypoxia, hypothermia, acidosis, N2O- any others? In regards to vasoactives, phenylephrine vs levophed when in CVOR? At what point would you consider giving something to decrease pulm pressures? NTG or SNP?
All of what you mentioned. I don’t routinely use phenylephrine in my practice (prefer vasopressin and norepinephrine), nor do I use NTG/SNP (prefer inhaled pulmonary dilators). Rest of my decisions are based on the nature of surgery, functional status, anticipated changes, intraoperative TEE findings, etc.