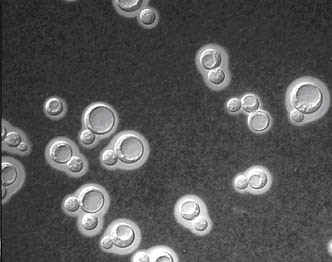
The meninges are layers of tissue which envelope the surface of the brain and spinal cord and carry a lot of the superficial vasculature which feeds the central nervous system. When these tissues become irritated or infected, the resulting inflammation is called meningitis. There are many infectious organisms associated with meningitis, but the purpose of this post is to explore cryptococcal (“crypto”) meningitis in the context of HIV/AIDS.
Most people with immunocompetent bodies have never heard of crypto, but once a person becomes immunosuppressed (namely with low CD4 counts due to HIV/AIDS), they can quickly start contracting opportunistic infections which are rare in the general population – CMV, pneumocystis, candida, and crypto to name a few.
A common symptom associated with cryptococcal meningitis is the extremely high lumbar puncture opening pressures which can be found in some patients (>200 mmHg H2O). This is usually one of the first keys in diagnosing a crypto meningitis, but the most reliable is the serum cryptococcal antigen and/or growth of the organism from the CSF culture. Treatment is usually two weeks of flucytosine and amphotericin B (amphoB).
An interesting note is that flucytosine and amphoB are typically contraindicated due to increased toxicities, but in the event of cryptococcal meningitis, dual therapy may actually be life-saving and is indicated in spite of the side effects. Flucytosine becomes metabolized into a product which interferes with fungal nucleic acid synthesis and amphoB basically “pokes holes” into the ergosterol membrane promoting the destruction of ion gradients. Some speculate that these holes also allow flucytosine to have better access into the organism. Also, in a lot of cases, protocol advises physicians to treat underlying opportunistic infections prior to beginning HAART on a newly diagnosed HIV patient for concern of throwing their body into immune reconstitution inflammatory syndrome (IRIS). Finally, cryptococcal meningitis patients are usually treated for life with fluconazole (in spite of improving CD4 counts after beginning HAART) because of the high frequency of relapse.
| AmBisome 3mg/kg | AmBisome 6mg/kg | AmphoB 0.7mg/kg | |
| n | 86 | 94 | 87 |
| Induction tx duration | 13.5 days | 14.0 days | 13.3 days |
| 2 wk culture conversion | 63.3% | 53.7% | 53.7% |
| 2 wk clinical response | 65.8% | 75.3% | 65.8% |
| 2 wk survival | 90.7% | 94.7% | 89.7% |
| Chills/rigors | 5.8% | 8.5% | 48.3% |
| Fever | 7.0% | 8.5% | 27.6% |
| Respiratory problems | 0% | 1.1% | 9.2% |
| Nephrotoxicity | 14.0% | 21.3% | 33.3% |
Dr. Richard Hamill of the Baylor College of Medicine and DeBakey Veterans Affairs Hospital assessed the efficacy of AmBisome versus conventional amphotericin B. Or as he likes to call it – “amphoterrible” (on account of its numerous “shake ‘n bake” side effects). The results have been compiled in the table above.1
It should be noted that AmBisome is just as effective as conventional amphotericin B but has significantly fewer side effects. Further studies (not shown) investigated using AmBisome in even higher doses due to the lower incidence of fevers, chills, rigors, etc.
All in all, crypto sure demands a lot of attention and treatment for immunocompromised patients.
1 AmBisome® Phase III Study For Cryptococcal Meningitis – https://www.gilead.com/pr_938462832





