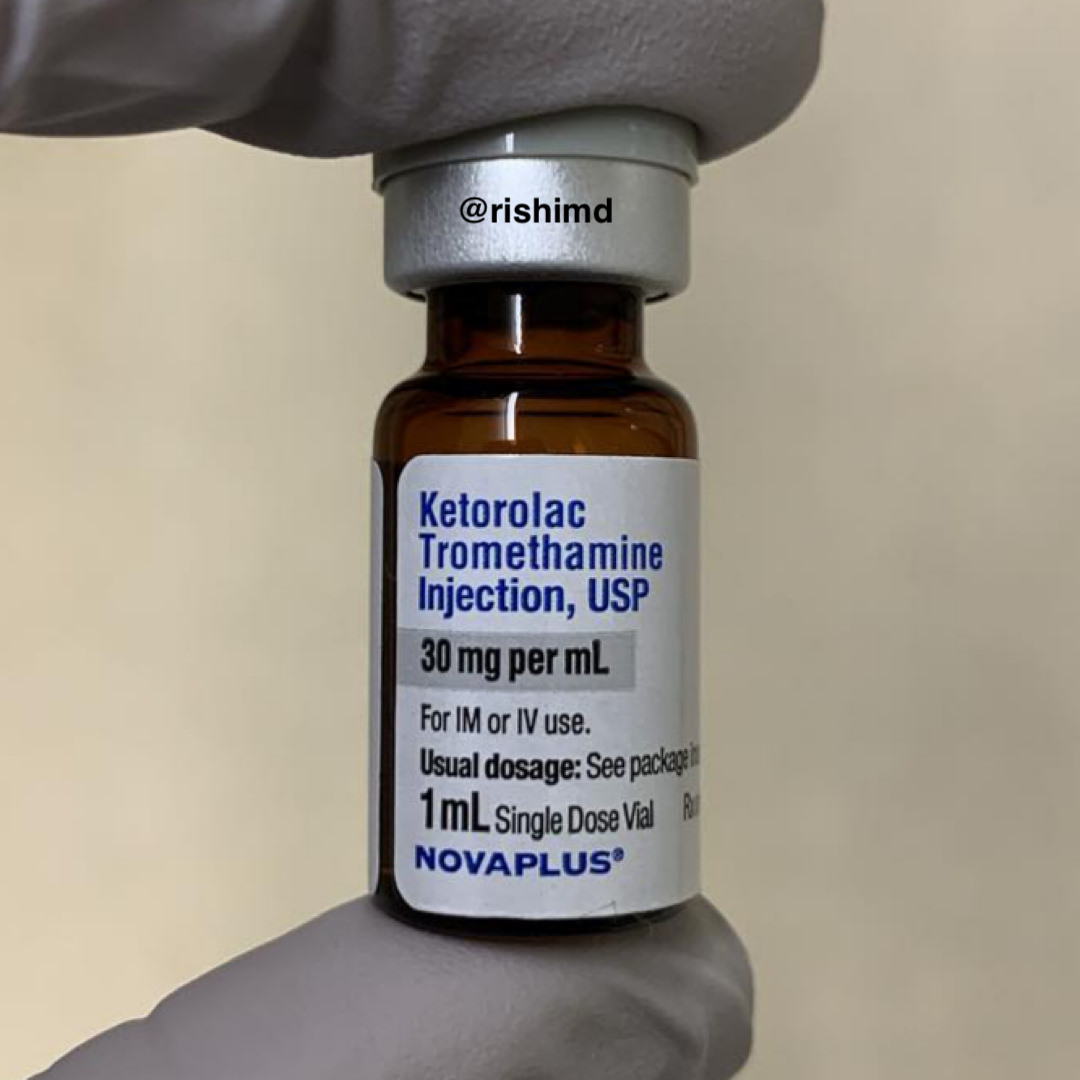
Ketorolac (Toradol) is a nonsteroidal anti-inflammatory drug (NSAID) I use as an analgesic adjunct in the OR and ICU. In some anesthesia texts, a single dose of IV ketorolac is said to confer analgesia equivalent to 10 mg of IV morphine (without narcotic-related side effects)! There’s some evidence from the EM world that suggests an analgesic “ceiling effect” at 10 mg of IV ketorolac. Beyond this dose, only more side effects are seen with no significant change in pain improvement. This is also my practice in the OR and ICU.
NSAIDs including ketorolac should be used cautiously in patients with kidney injury as they inhibit prostaglandins which are normally responsible for regulating flow through the afferent renal arterioles. Furthermore, COX-1 inhibition can lead to gastric ulcerations due to changes in the mucosal barrier defense mechanisms.
Interestingly, although NSAIDs are typically associated with bleeding, the risk of thrombosis in post-coronary artery bypass grafting (CABG) patients is a specific concern raised by an FDA black box warning. This can be attributed to an imbalance in COX-1 and COX-2 inhibition. COX-1 normally results in thromboxane A2 synthesis – a potent platelet aggregator (pro-thrombotic). COX-2 creates the antithrombotic prostaglandin I2. Inhibition of COX-1 and COX-2 can, therefore, result in bleeding and clotting, respectively.
For the aforementioned reasons, it’s important to consider the COX-1 and COX-2 inhibitory properties of all NSAIDs. While selective COX-2 inhibitors (ie, celecoxib) may be beneficial in terms of minimizing bleeding and gastric ulceration, they may also lead to a higher risk of thrombosis.
Drop me a comment below with questions! 🙂