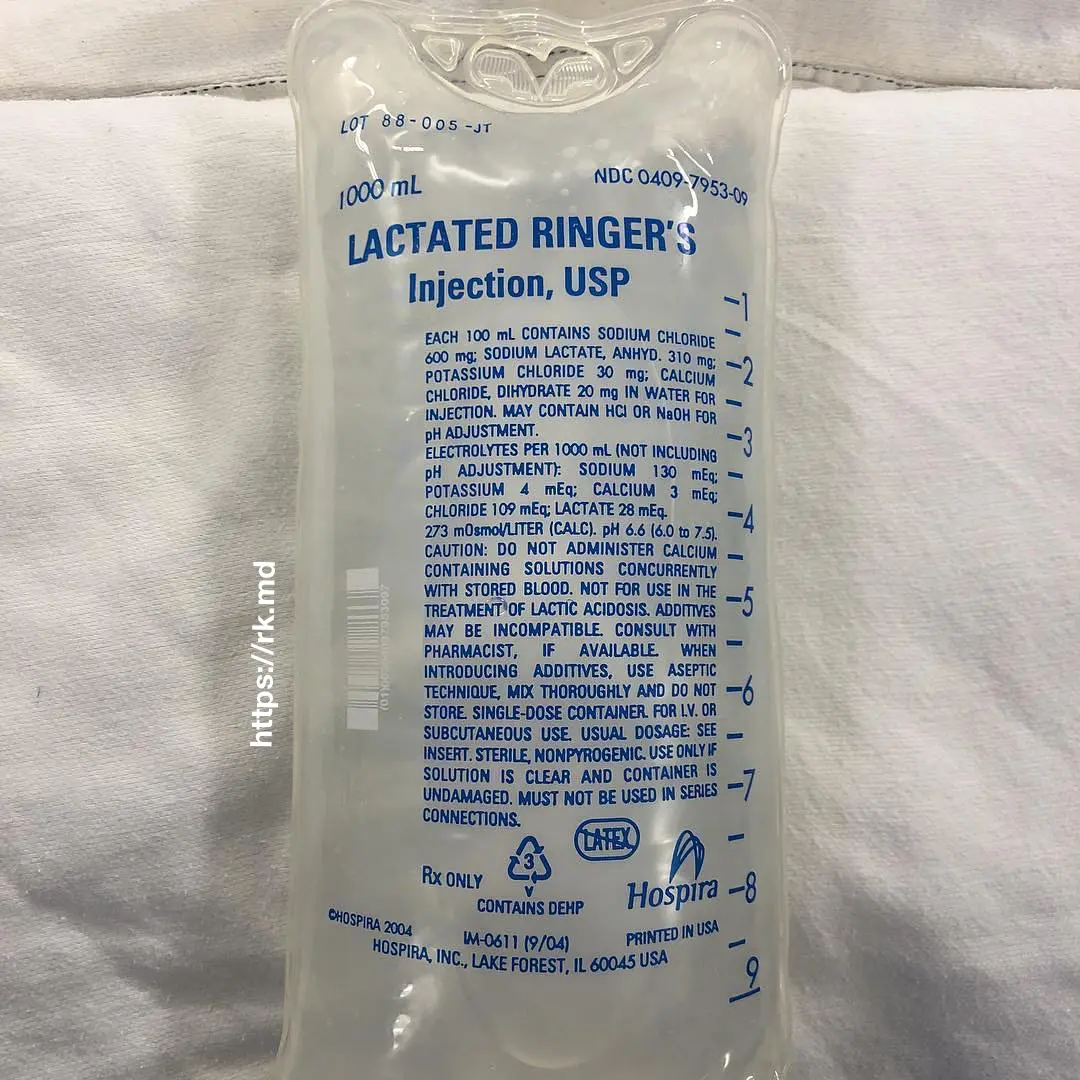
Lactated Ringer’s (LR) is a balanced crystalloid solution created by Dr. Sydney Ringer in the 1880s using ex-vivo frog hearts. It contains sodium, chloride, lactate, potassium, and calcium, yielding an osmolarity of 273 mOsm/L (human plasma is ~ 290 mOsm/L). In the OR and ICU, I preferentially use balanced crystalloids like LR over saline in most cases as a resuscitation fluid.
LR provides some degree of intravascular volume expansion in addition to sodium lactate – a substrate that can generate bicarbonate equivalents with oxidative metabolism. Remember that ongoing resuscitation to promote adequate delivery, uptake, and utilization of oxygen is still necessary to clear lactate produced endogenously.
There is some controversy about using LR in patients with hyperkalemia (> 5.5 mEq/L); however, due to potassium’s volume of distribution being larger than the extracellular fluid compartment and equilibration between the intra/extracellular compartments, potassium levels will trend DOWN towards 4 mEq/L (the K+ concentration in LR). Also, these patients tend to be acidotic. A saline (chloride) load can potentially complicate matters with a superimposed non-anion gap, hyperchloremic metabolic acidosis.
Last, remember we are not infusing lactic acid. Sodium lactate can be used as a fuel by organs like the heart, producing bicarbonate equivalents (see aforementioned). However, LR can affect lactate lab values which I often assess in the OR and ICU.
Drop me a comment below with questions! 🙂






Would you still use LR for kidney transplant cases or pt w/ ESRD? Also what about for liver transplant cases or pt w/ ESLD? At my hospital, we use NS or Plasmalyte. I guess we could use LR for kidney cases given the above explanation about K’s Vd. Thank you.
To avoid ruffling feathers, I’ll stick with protocols after transplant cases (saline). Keep in mind that Plasmalyte has even more potassium than LR (5 mEq/L vs 4 mEq/L, respectively). No substitute for just letting the patient eat/drink though! 🙂