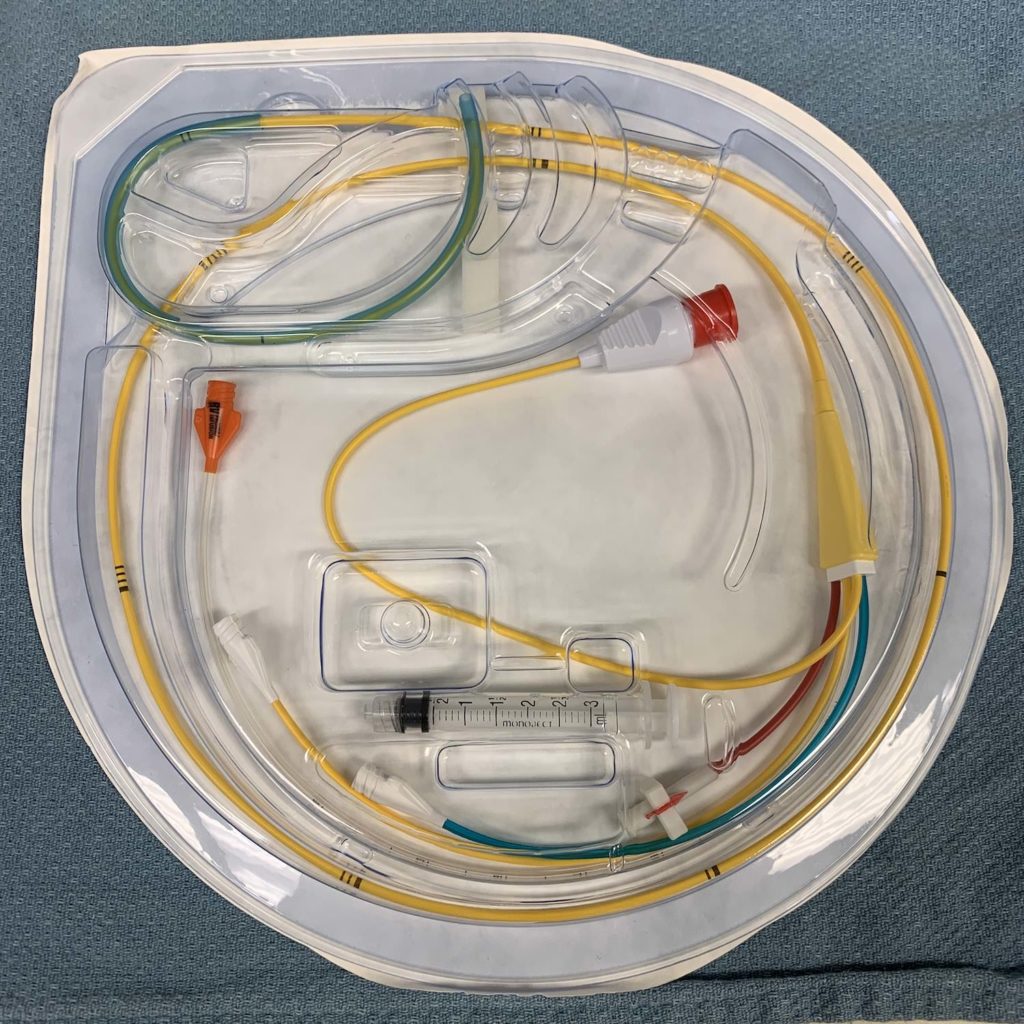
Throughout my training, I’ve placed countless pulmonary artery (“Swan-Ganz”) catheters for cardiothoracic surgeries and in the ICU to help guide the diagnosis and response to therapy in mixed or undifferentiated shock. These PA catheters gave me various pressures (central venous, pulmonary artery, sometimes right ventricular), the ability to draw true mixed venous gas samples, and a continuous cardiac output (CCO).
I’ve also had the opportunity to place a special kind of PA catheter – the pacing Swan. There are many ways to “pace” the heart – endocardial wires (as seen with pacemakers), epicardial wires (often placed after cardiac surgery), tranvenous wires, transcutaneously (please provide some sedation!), and even via the transesophageal route.
Sometimes during cardiac surgery when it’s technically challenging to place an aortic cross clamp and epicardial wires, the surgeon may elect to perform hypothermic fibrillatory arrest for myocardial protection rather than the conventional cardioplegic arrest. Fibrillation prevents the heart from ejecting blood and allows the surgeon to operate in a relatively “motionless” field while coronary perfusion is maintained.
As a cardiac anesthesiologist, I can facilitate this process with a pacing Swan. These devices are “floated” into the pulmonary artery much in the same way I place traditional Swan-Ganz catheters with transesophageal echocardiography (TEE) and/or pressure transduction; however, the pacing variant has additional ports that can provide atrial pacing, ventricular pacing, or A-V sequential pacing in addition to cardiac output measurements with the thermodilution technique. Once the catheter is properly positioned, I simply connect the ventricular lead to a pulse generator, and bam, ventricular fibrillation!
Drop me a comment below with questions! 🙂


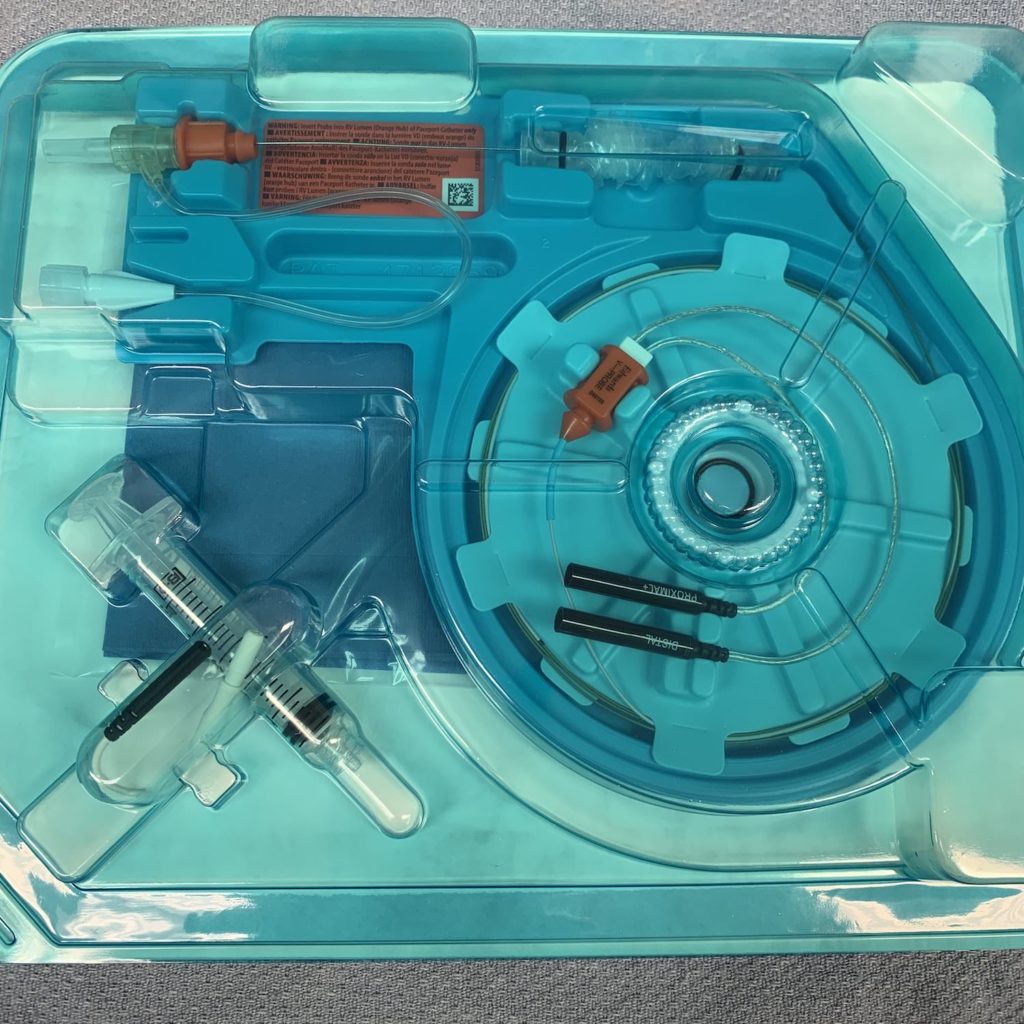




Hey rishi, how can this type of swan ganz catheter have a DDD pacing mode. You can just advance only 1 wire through the orange (middle) port. You normally need 2 sets of wires for DDD unless there is another way with these catheters. Also if you don’t have this catheter and just a normal swan, in order to pace you have to remove the swan and insert a normal pacing wire through the cordis right? Thank you for your time!
Great question, Kostas! I’ve only done VVI pacing through these Swans because, as you alluded to, it’s only going to give you the equivalent of a single RV lead. More often, I’ve fibrillated the heart through this Swan by connecting it to a fibrillator box for the purpose of cold fibrillatory arrest during surgery. And if you wanted to do more conventional transvenous pacing, yes, you’d remove this Swan versus getting a secondary venous access (e.g., “double-sticking” the internal jugular vein).
Hello Dr Rishi,
I am a physical therapist that works in a cardiac intensive care unit and I came across a pacing PAC in one of my CABG patients. I know research shows that mobilizing PACs is safe but I have not come across any literature regarding mobilizing patients with these types of PACs. Do you have any recommendations? Same as normal PAC or are there any precautions/contraindications.
Thanks!
Hey Matt! I’m so glad you found data in favor of mobilizing patients with PACs. I think many hospitals adopt a culture where they shy away from this, and in the process, put patients at higher risk for things like venous thrombosis, less pulmonary recruitment, etc. As far as PACING PACs go, I really don’t know the data. For temporary pacers like epicardial pacing wires or pacing PACs, I’d imagine the concern would be dislodging the leads. If a patient is DEPENDENT on pacing, I’d naturally be more reluctant, but if they’re just serving as a backup, I’d reinforce the leads (ie, making sure the pacing PAC is secured well), and ambulate away! I’d love to know what other people think!
Hi, dr. Rishi
How does it get into pulmunary artery?
How do you know it’s not coiling as you advance?
How you going to know whether this truly pulmunary artery or whether is blow up?
Be blessed
Luz sapnu
A small balloon at the tip is inflated allowing the catheter to be carried along with the blood flow into the right atrium → right ventricle → and then pulmonary artery. It often times DOES coil, so experience is important. Also, I can sometimes see the catheter coiling in the right atrium or right ventricle with transesophageal echocardiography (TEE).