Calcium is traditionally reported as a total serum concentration (i.e., complete metabolic profiles) and ionized calcium concentration (i.e., blood gases). To interpret these labs, one must understand what they represent. Under normal physiologic conditions, roughly 50% of calcium is bound (primarily to albumin), and 50% is ionized (the biologically active component). Therefore, total calcium = bound + ionized.
Based on this relationship, it’s possible to see an increase/decrease in total calcium WITHOUT a change in ionized. This is the premise behind “pseudo-hyper/hypo-calcemia,” which is largely driven by changes in albumin concentration. More recent literature has shown that the “albumin correction formula” (corrected [Ca] = 0.8 * (4 – [albumin]) + measured [Ca]) provides poor estimates in the critically ill/renally compromised patient populations, so use it mindfully!
Ionized fractions can also change without affecting the total calcium concentration! In the OR and ICU, I see this in the context of acid-base derangements. Albumin is a negatively charged protein that attracts positively charged calcium ions AND H+ ions (pH). In acidotic states, [H+] increases and competes with calcium to bind albumin. Thus, less calcium has a home on albumin, and more is left ionized in its biologically active state. Since this represents a shift between bound and unbound states, the TOTAL remains relatively UNCHANGED.
As a cardiac anesthesiologist and intensivist, I’m almost invariably looking for ionized calcium to guide therapy, electrolyte repletion, etc. Why? Because this tells me what I need to know – the biologically active fraction! In lower-risk patients… well… please don’t send extra labs unless you’re going to DO something with them!
Drop me a comment below with questions!






I am curious about a diagnosis of hyperparathyroidism. My PTH was elevated, 140, my calcium was normal; however, my potassium was elevated to 7.1. Nuclear scan noted nothing but the endocrinologist said he is sure I have an adenoma on my parathyroid. He did exploratory surgery and removed three of my parathyroids. This was ten years ago. I am having symptoms and an elevated PTH with all other labs normal. I am wondering what is the link between parathyroid hormone and potassium. I did not inquire at that time because I was not familiar but am now curious and so is my present doctor.
I have been diagnosed with hyperparathyroidism/ hypercalcemia. My serum calcium has been coming in at high normal to high (average 10.6) for several years. PTH is often double that of the high normal. Because the levels weren’t extremely indicative to proceed with surgical exploration, we have been “monitoring” only the serum calcium level. Finally upon my insistence, I asked the endocrinologist to obtain the ionized calcium level. So here’s a recent measurement: serum @ 9.9, ionized @ 5.8, PTH @ 132. I do have severe acidosis and tinnitus, calcifications forming in my liver and spleen, on my kidneys and lungs, some signs of atherosclerosis, mild osteopenia, anxiety, depression, memory loss, and vision problems. A recent consultation with an endocrine surgeon demonstrated through ultrasound that I have at least one enlarged parathyroid gland the size of a grape. Do endocrinologists understand the importance of knowing the balance of bound to unbound calcium? I am finding that they don’t and that it does cause more harm to the organs to ignore the ionized ratio especially over longer periods of time. Anion gap was also being dismissed as anomaly. Waiting for renal failure or osteoporosis is too late. Please emphasize this to the old school.
Thanks for sharing your experience. Yes, I’d say that endocrinologists know the importance of everything you mentioned. Anion gaps can certainly be difficult to interpret with an increased in unmeasured cations (calcium in this case).
What level of ionized calcium do you treat? I’m a CICU RN and I push to treat under 1.05 ionized calcium. Usually I meet resistance from doctors to treat those levels and I never have a good enough argument to tell them why they should lol.
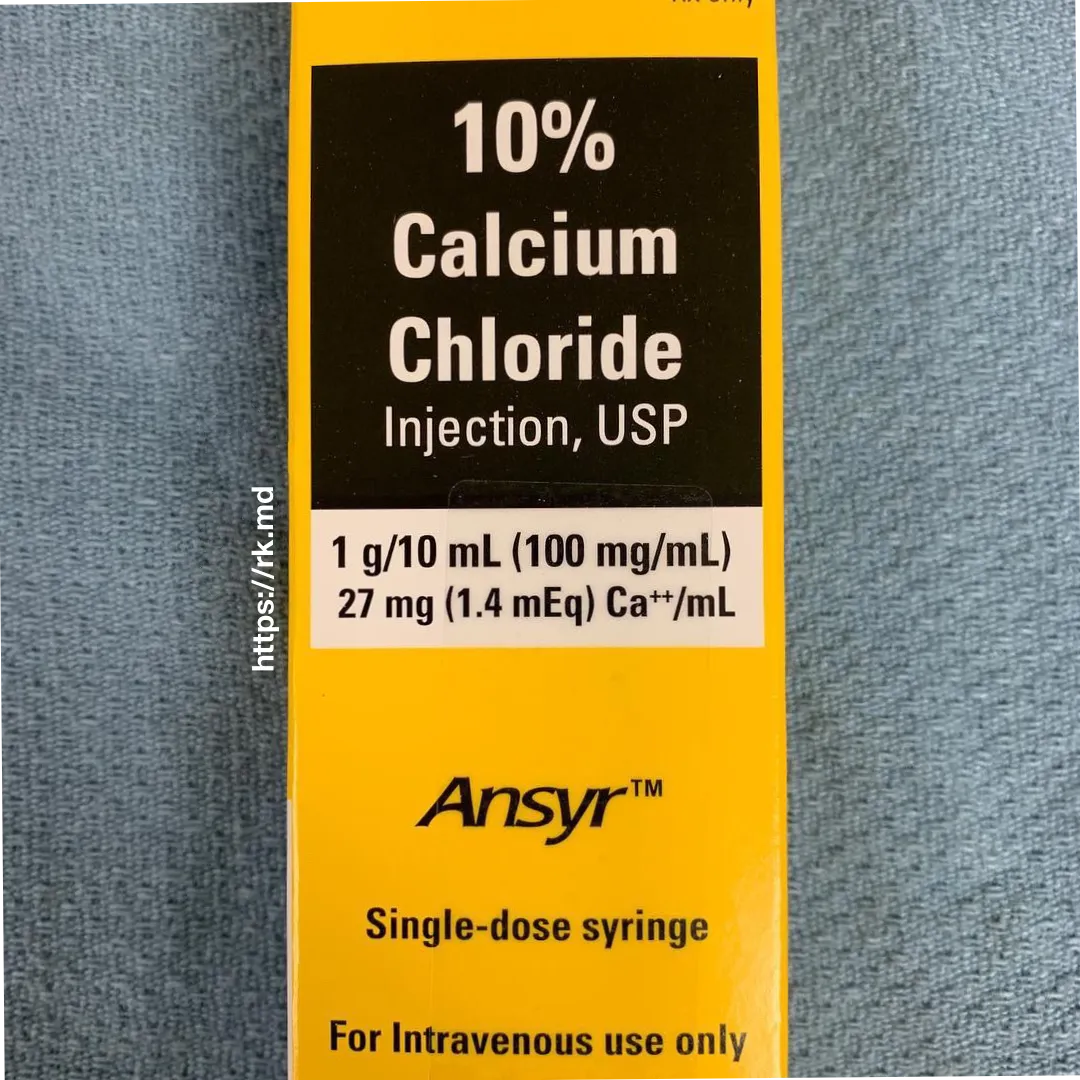
Cardiac anesthesiologists LOVE calcium! In the context of a large surgery (especially if I’m struggling with coagulopathy, low systemic vascular resistance, or contractility issues), I have a very low threshold to give calcium for ionized < 1.1.
Why then is the lab reported as ionized calcium and then below it is listed the normalized calcium, I do not know what to do with this and can’t remember when it started be reported this way. Sometimes the ionized is slightly high but then the normalized calcium is normal. For example 1.53 (high ionized) vs 1.31 ( normal normalized).
Hmmm, I’m not sure what a “normalized” calcium is in this context! Our labs/ABGs give calcium as either ionized or total, so that’s what I referenced in my post.
Thank you! Very helpful.
You’re very welcome! 🙂