Removing an endotracheal tube and ventilator support from a patient nearing the end of life (“terminal extubation”) is a decision reached by family members/decision-makers with the support of ICU staff and/or organ procurement organizations for organ donation after circulatory death (DCD). The body’s response to dying generates some common hemodynamic changes.
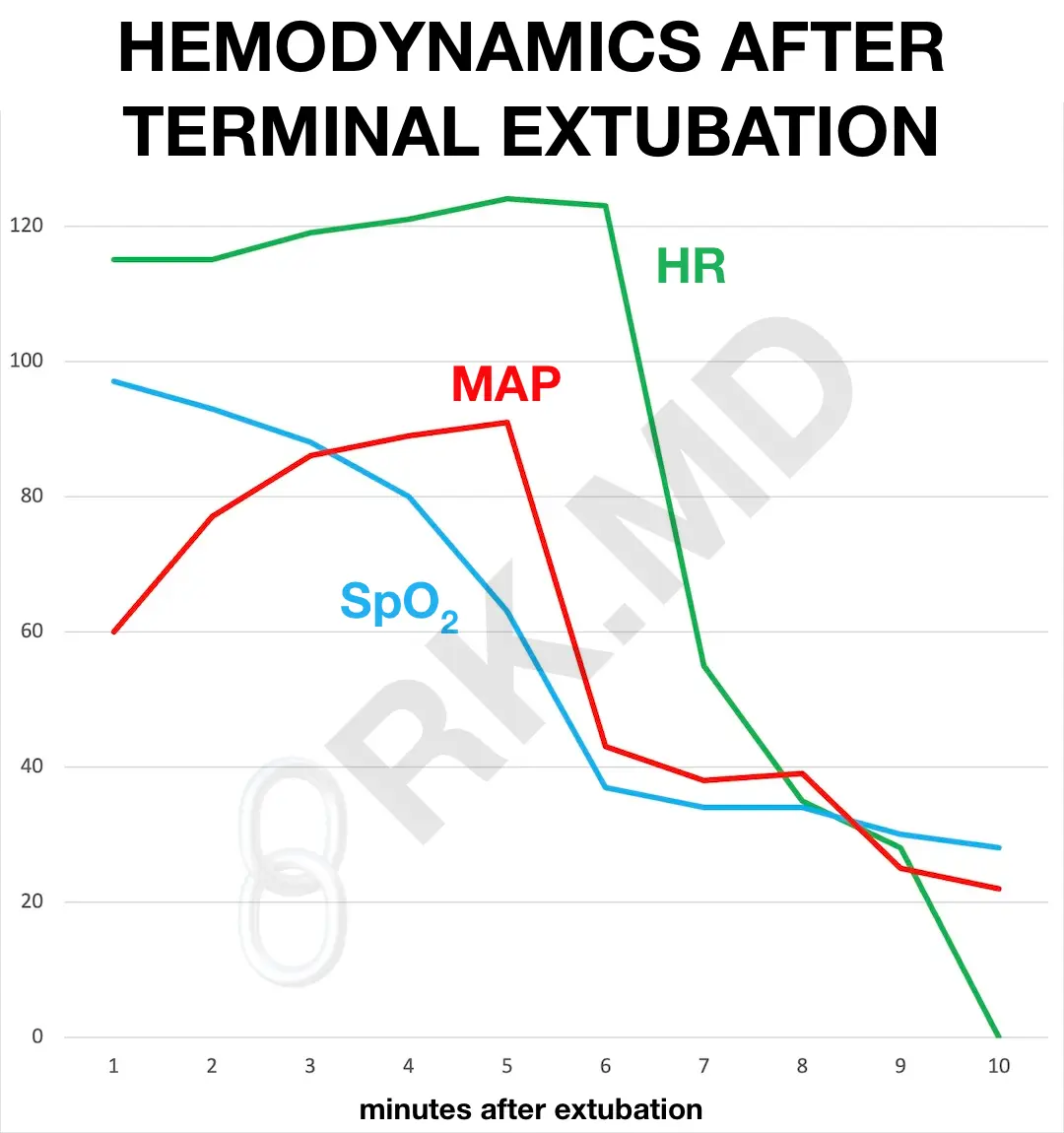
In the pictured vitals, terminal extubation is at time 0. Irregular and shallow breathing patterns will lead to hypoxemia (↓ “pulse ox” SpO2) and hypercarbia (↑ arterial carbon dioxide). A sympathetic surge can increase the heart rate (HR), cardiac output, and mean arterial pressure (MAP). However, hypotension and bradycardia will follow as the body’s energy reserves diminish and hypercarbia with associated acidemia sets in. As the body tries to maintain blood flow to vital organs, peripheral vasoconstriction may occur, leading to mottled and cyanotic extremities.
Eventually, the metabolic derangements from reduced oxygen delivery will cause the heart to stop. At this point, I will perform an exam and pronounce the patient dead. Specifically, in the case of DCD, I’ll often be the one to bring the patient (who we term “hero” due to their selfless donation of organs to save other lives) to the operating room, re-pronounce, and then the procurement process will begin.