In the perioperative arena, the terms “MAC” (monitored anesthesia care) and “sedation” are used interchangeably; however, they are not the same. The term MAC has nothing to do with levels of sedation (minimal, moderate, deep, and general anesthesia).
As described by the American Society of Anesthesiologists (ASA):
Monitored Anesthesia Care (MAC) does not describe the continuum of depth of sedation, rather it describes “a specific anesthesia service in which an anesthesiologist has been requested to participate in the care of a patient undergoing a diagnostic or therapeutic procedure.”
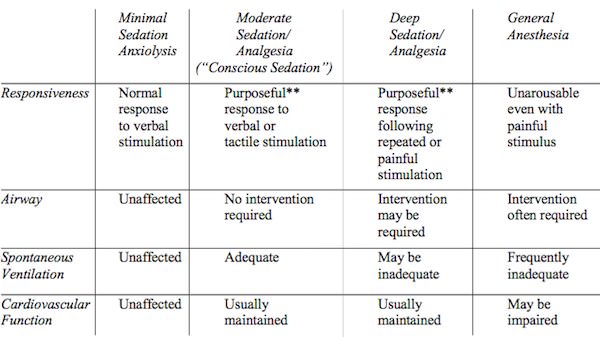
The ASA has also released the “Continuum of Depth of Sedation: Definition of General Anesthesia and Levels of Sedation/Analgesia.”
There is no “right” medication or dose for any given situation either. For example, one can run a propofol infusion at varying doses to achieve any of the aforementioned levels of sedation. Personally, I use agents like propofol, remifentanil, ketamine, fentanyl, midazolam and dexmedetomidine for MAC cases. The MAC provider must be prepared to convert to a general anesthetic at any point during the procedure and rescue the airway from compromise.
Take home message: the depth of sedation is defined by the patient’s responsiveness to stimuli and how their cardiopulmonary status is affected.
Drop me a comment below with questions! 🙂






Hello Rishi! My questions may seem stupid. How do I know that a patient in the ICU is sedated without the staff telling me? Can I assess patient’s neurological status without sedation interruption?
Hey Sarah! Not a stupid question at all. I use scoring systems like the Richmond Agitation and Sedation Scale (RASS) to determine to what extent my patients are sedated (with or without pharmacologic therapy) and communicate what my goal is (usually -1 to 0). You can certainly do this without interrupting sedation; however your score will very likely be lower. If you’re trying to determine what patients are doing at baseline, then yes, you would absolutely need to wean the influence of pharmacologic therapies.
Thank you Rishi for your comments. I have been debating your thoughts and recommendations and have considered them very seriously before I meet with the Anesthesiologist tomorrow who is to administer my anesthesia.
What length for MAC do you consider safe and that you would be comfortable with delivering personally yourself?
Is it at all possible to have a MAC anesthesia with the sole anesthetic agent being remifentanil delivered with a TCI system.
Also, here is a statement from a NCBI article titled Propofol in Office-Based Plastic Surgery—
differences in propofol response make measurement of the target organ (i.e., the brain) with a bispectral index (BIS) monitor very important. BIS levels 1 hour are associated with increased 1-year anesthesia mortality thought to be associated with an inflammatory response. The only currently available way to avoid overmedicating with propofol is to monitor with a level of consciousness monitor like BIS.
Overmedicating can produce deeper than intended levels of sedation and has now been shown to be undesirable.12,15 The BIS monitor must be considered a standard of care when propofol is being administered
Does this concern you about the potential inflammation of the brain secondary to Propofol with resultant neuronal apoptosis and resultant cognitive dysfunction, which the literature indicates is 37% in patients over the age of 60? Thanks, Don
Hey Don! Hopefully the procedure went well! I don’t really have a time frame for what I consider “safe” MAC anesthesia as this is largely determined by patient and surgical factors which vary from case-to-case.
Remifentanil is a pure narcotic, and I’d surmise at doses high enough to achieve a deep sedation, respiratory compromise may ensue. BIS is just a surrogate for “awareness.” I don’t use it that often since I tell patients that they might actually be aware of voices, etc. during MAC (and that’s totally okay).
I really haven’t heard about these inflammation concerns surrounding propofol, but quite frankly, avoiding side effects is one of the reasons why I often use balanced MACs (multiple agents in low doses) for longer cases.
I am contemplating an elective plastic surgery procedure to include upper and lower blephroplasties and facial structural fat grafting. which the surgeon says will take 4 to 5 hours.
I am a surgeon myself and have training in anesthesia as well. It is to be done with MAC anesthesia. I want to reduce the exposure to propofol and can not take benzodiazepines.
I have suggested that we do the upper blephroplasty and fat graft harvesting using local anesthetic, Ketamine and fentanyl or Dilaudid then add a propofol infusion to finish the lower blephroplasty and structural fat grafting. I would think this could reduce the propofol exposure to approximately 2 hours. Does this sound like a feasible anesthesia approach?
Hey Don! Honestly, I’ve always kept my MAC anesthetics as simple as possible with infusions like propofol and remifentanil with plenty of local anesthetic to cover immediate post-operative pain. The more I venture into mixing agents (especially things like ketamine), the less predictable I find the anesthetic course. And this is coming from someone who routinely uses ketamine in general anesthetics and basic procedures like chest tube placement.
I’m not going to tell you what route to take, but if this was me, I’d definitely just opt for a propofol +/- remifentanil infusion. 4-5 hours also sounds awfully long for a MAC case, so there’s that consideration too.