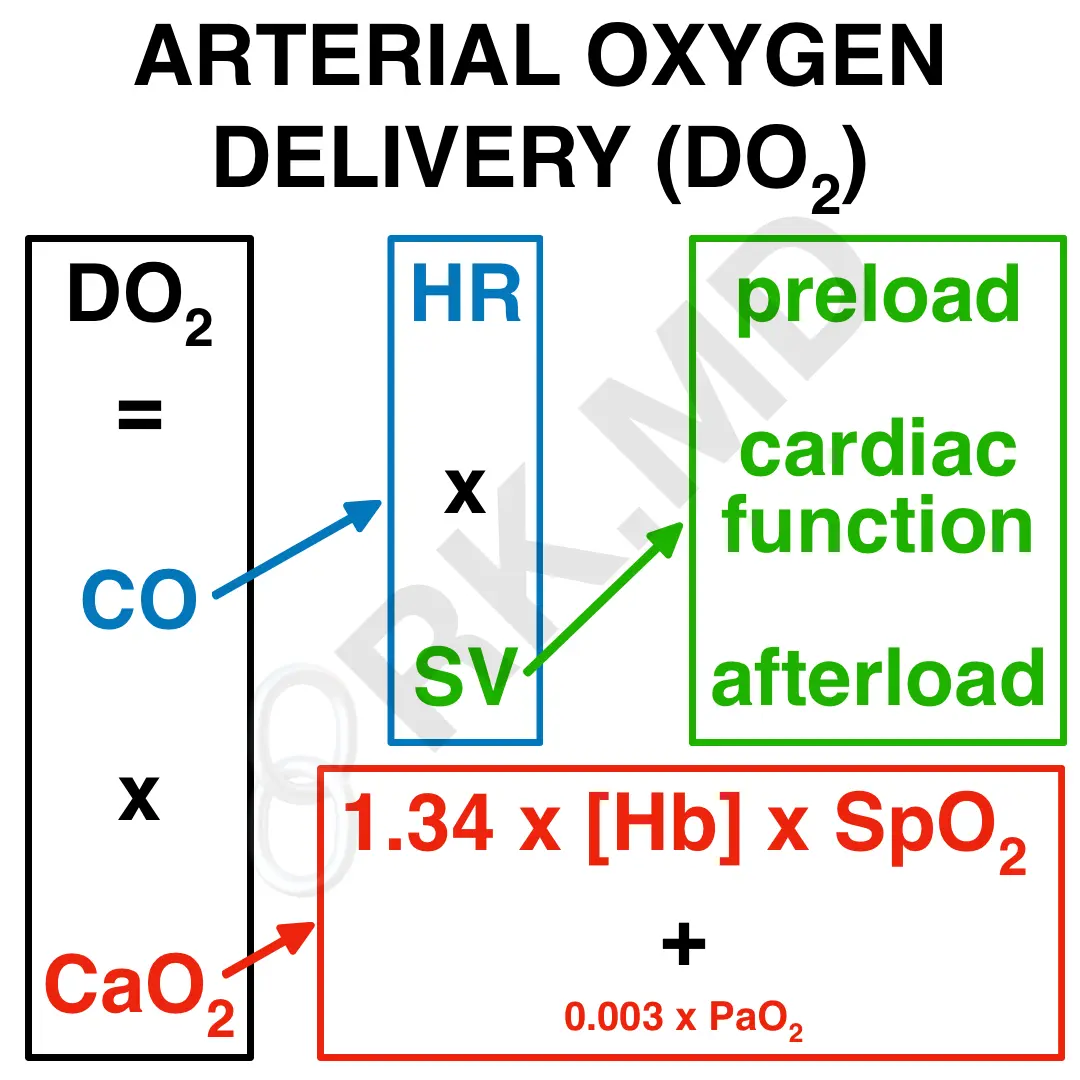
The arterial oxygen delivery (DO2) equation is undeniably one of the most essential physiologic principles. DO2 is comprised of two variables:
- Cardiac output (CO): This is the product of heart rate (HR) and stroke volume (SV), or the volume of blood ejected with each beat. SV is, in turn, related to cardiac preload (venous return), cardiac function (contractility, relaxation, etc.), and afterload (resistance to forward flow).
- Arterial oxygen content (CaO2): The sum of (1.34 x [Hb] x SpO2) and (0.003 x PaO2), the latter of which normally contributes very little to the overall CaO2 due to the 0.003 multiplier. [Hb] is the hemoglobin concentration, SpO2 is the arterial oxygen saturation (as a decimal), PaO2 is the partial pressure of oxygen in the blood (derived from an ABG).
It’s crucial to consider acute changes (e.g., hemorrhage and desaturation) in the context of this equation. As shown, hemoglobin concentration and the oxygen saturation of that hemoglobin are the most critical determinants of CaO2. A patient can saturate 100% of their hemoglobin, but if the [Hb] is only 4 g/dL, the oxygen content will be very low due to profound anemia. These patients will rely more on the partial pressure of oxygen (PaO2) to augment their overall O2 content until a red cell transfusion is performed.
Once the CaO2 is optimized, it’s a matter of improving the patient’s cardiac output (CO) to facilitate oxygen delivery. Again, it is crucial to know how a patient’s comorbidities and clinical context affect their preload, cardiac function, afterload, stroke volume, and heart rate/rhythm, as these are the modifiable parameters to improve cardiac output.
The next time you’re reassured that a patient is “satting 100% on room air”, remember to think about their actual oxygen delivery rather than being reassured by a single number. 🙂