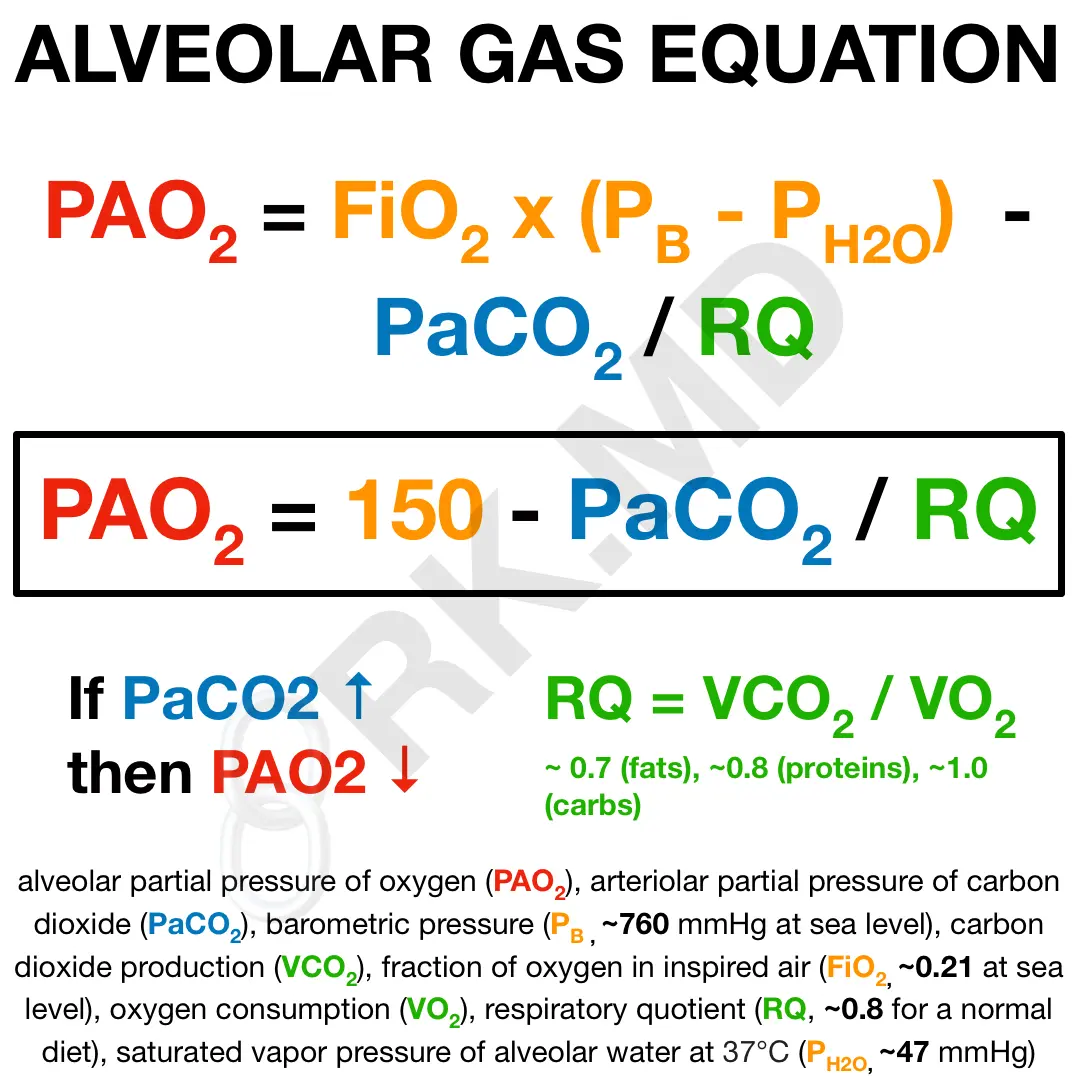
I previously wrote about the oxygen delivery equation mathematically describing a vital concept in physiology. Now I want to discuss another critically important formula in acute care medicine – the alveolar gas equation.
The most important relationship shown by this equation is that as arterial carbon dioxide (PaCO2) increases, the alveolar partial pressure of oxygen (PAO2) must decrease. This implies that worsening hypercarbia will ultimately lead to hypoxemia.
Additionally, decreasing the inspired oxygen concentration (FiO2) or increasing the altitude (decreased barometric pressure, PB) will also reduce PAO2 independent of PaCO2.
As an intensivist and cardiothoracic anesthesiologist, I utilize this equation (for alveolar oxygen, PAO2) in combination with arterial blood gas (for arterial oxygen, PaO2) to determine how effectively oxygen is being transferred into the bloodstream for my patients in the ICU and OR. The resulting “A-a” gradient helps me determine the cause(s) of hypoxemia.
Normal A-a gradient (5-10 mmHg): I’m thinking of either hypoventilation (poor pulmonary mechanics, neuromuscular disease/weakness, CNS depression from sedation, etc.) or ↓ FiO2 due to high altitude.
Elevated A-a gradient: I’m thinking of pathologies that create ventilation-perfusion (“V/Q”) mismatch, right-to-left shunts (e.g., intracardiac defects like ASD/VSD, pulmonary arteriovenous malformations, etc.), diffusion defects across the alveolar-capillary membrane interface like fibrosis, and hypermetabolic states with high oxygen consumption.
Understanding the alveolar gas equation is important to know if a patient’s oxygenation and ventilation make sense based on measured lab values, and how we can go about optimizing variables to improve these parameters. 🙂






What are your thoughts on pulmonary edema? Some texts say that increasing FiO2 will not increase PAO2 because of it’s right-to-left shunt properties.
In theory, yes I agree. But it’s not practical to sample the PAO2 from alveoli throughout the lung to determine the extent to which this is true. Furthermore, when you factor in things like oxygen itself being a pulmonary dilator, the effects/disruption of hypoxic pulmonary vasoconstriction, prior cardiopulmonary comorbidities, and co-existing shunts… it gets complicated. 😃
With all that said, clinically, if a patient has full blown pulmonary edema with hypoxemia, increasing supplemental oxygen is absolutely on my list of therapies to try.