Understanding mechanical ventilation is a fundamental part of intensive care and perioperative medicine. Here’s an overview of the basics. Keep in mind that clinically, there are many more things to consider, exceptions to rules, hybrid ventilator modes, and other strategies that I will not cover for the sake of maintaining simplicity. Please leave me questions in the comments section at the bottom!
LOAD
For air to flow into the lungs, pressure must be delivered to overcome the resistive forces of the airways and expand the lungs/chest wall. In order for air to flow into the lungs, the pressure generated by the patient’s respiratory muscles (Pmus) coupled with the inspiratory pressure of the ventilator (Pvent) must exceed the sum of the resistive load (flow x airway resistance) and elastic load (elastance x volume). In other words:
Pmus + Pvent = (V̇ x R) + (E x V)
It’s essential to understand how a breath on the ventilator is initiated and terminated by phase variables (trigger, limit, cycling).
TRIGGER
A trigger dictates what causes the ventilator to cycle to inspiration. Modes can also have more than one trigger.
- Pressure-triggered: the patient generates negative pressure from diaphragmatic contraction
- Volume-triggered: the patient inspires a small volume of air from the ventilator
- Flow-triggered: the patient generates a small amount of airflow into their lungs
- Time-triggered: a preset timer dictates how often the patient breathes
LIMIT
A limit restricts a variable before the end of inspiration.
- Pressure-limited: a pressure that will not be exceeded during inspiration
- Volume-limited: a volume that will not be exceeded during inspiration
- Flow-limited: a flow rate that will not be exceeded during inspiration
CYCLING
The cycling variable dictates how the ventilator “cycles” between inspiration and passive expiration.
- Pressure-cycled: after achieving the peak inspiratory pressure (PIP), exhalation occurs
- Volume-cycled: after the target volume is delivered, exhalation occurs
- Flow-cycled: exhalation occurs when the inspiratory flow rate falls below a preset threshold
- Time-cycled: purely based on time
COMPLIANCE
The chest wall and the lungs are in a constant “tug-of-war” – the lungs want to collapse inward, and the chest wall wants to expand outward. These two systems work together to influence respiratory mechanics. Compliance is defined as Δ volume / Δ pressure. In other words, a stiff system (low compliance) requires lots of pressure (large Δ pressure) to drive in a small volume of air (small Δ volume). Examples of poor compliance include interstitial pulmonary fibrosis, pneumonia, acute respiratory distress syndrome (ARDS), etc.
OXYGENATION AND VENTILATION
The lungs provide oxygen (O₂) and remove carbon dioxide (CO₂) from the blood. These processes refer to oxygenation and ventilation, respectively. Oxygenation can be improved by increasing the fraction of inspired oxygen (FiO₂) and positive end-expiratory pressure (PEEP). PEEP helps maintain alveolar recruitment between respiratory cycles and is often increased concurrently with FiO₂.
Minute ventilation is the product of respiratory rate (RR or ‘f‘) and tidal volume (VT). Increasing either of these parameters will increase minute ventilation to remove more CO₂.
I/E RATIO
The inspiratory to expiratory ratio (I:E) refers to the time spent in each respiratory cycle phase. Under physiologic conditions, we usually spend 2-3 times as much time in passive expiration (I:E of 1:2 or 1:3). For example, if a patient is deeply sedated or paralyzed, they will breathe at the RR set on the ventilator. Let’s assume this is at 15 breaths/minute. That means a complete inspiratory-expiratory cycle lasts 4 seconds. An I:E ratio of 1:3 means that inspiration will last 1 second and expiration will last 3 seconds.
If this ratio changes to 1:1, then equal amounts of time are spent in inspiration and expiration. Inverse ratio ventilation occurs when more time is in inspiration than expiration (i.e., 2:1). This ventilation mode can be very uncomfortable and lead to “breath stacking” as there is inadequate time to exhale the previous VT. This can, in turn, lead to progressively higher mean airway pressures (the expiratory flow does not return to 0 L/m before inspiration) and alveolar trauma.
Now let’s talk about different modes of ventilation!
ASSIST CONTROL (A/C)
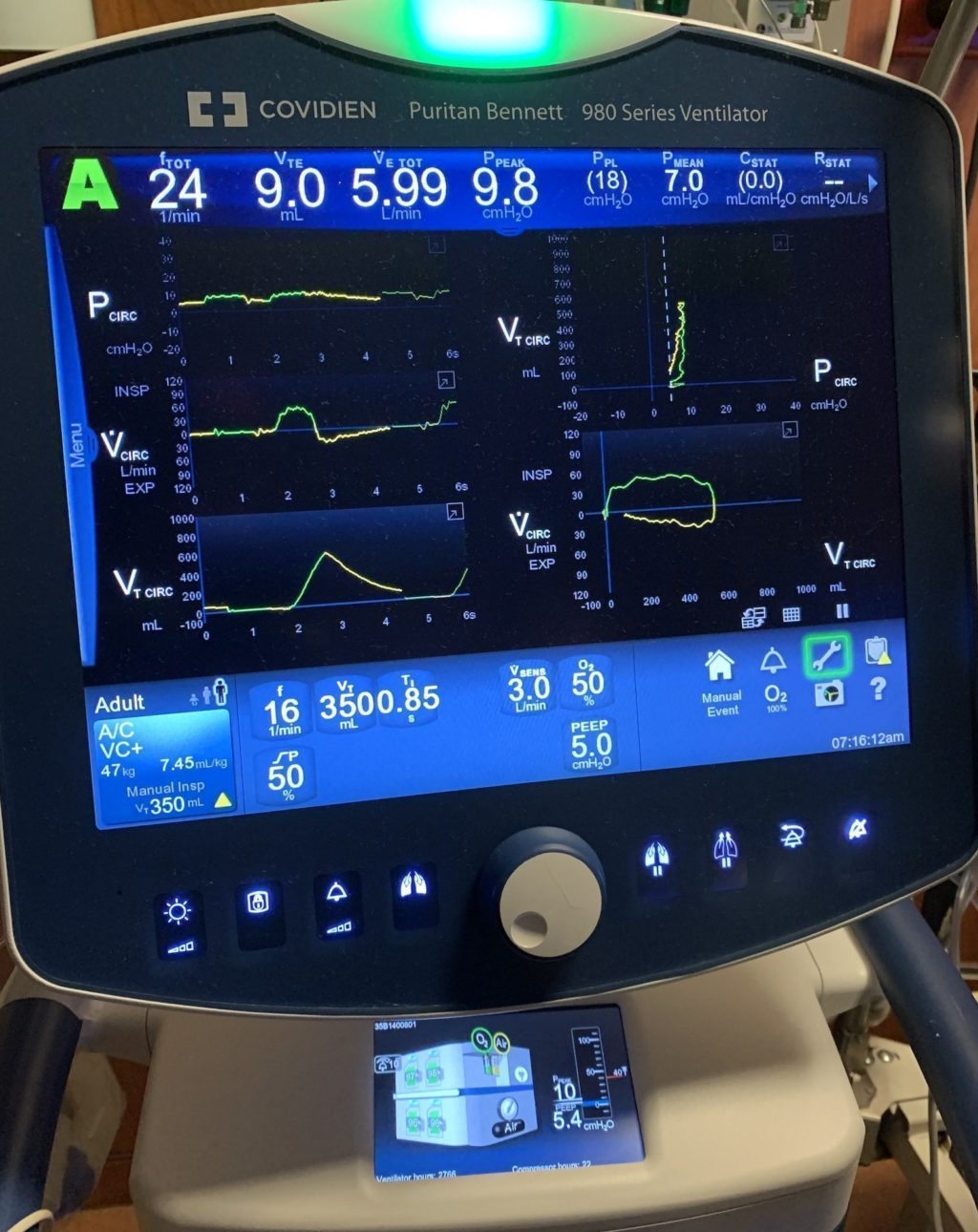
Assist control (A/C) is routinely utilized as a “rest mode” where the ventilator takes on the role of breathing (“control”). If the patient wants to breathe over the set RR, they can “assist” with ventilation. Therefore, if the patient does not trigger any breaths, the ventilator will achieve the preset minimum. For example, in the image above, the A/C mode (volume control) settings are: RR 16 bpm, VT 350 cc, FiO₂ 0.5, and PEEP 5 cm H2O.
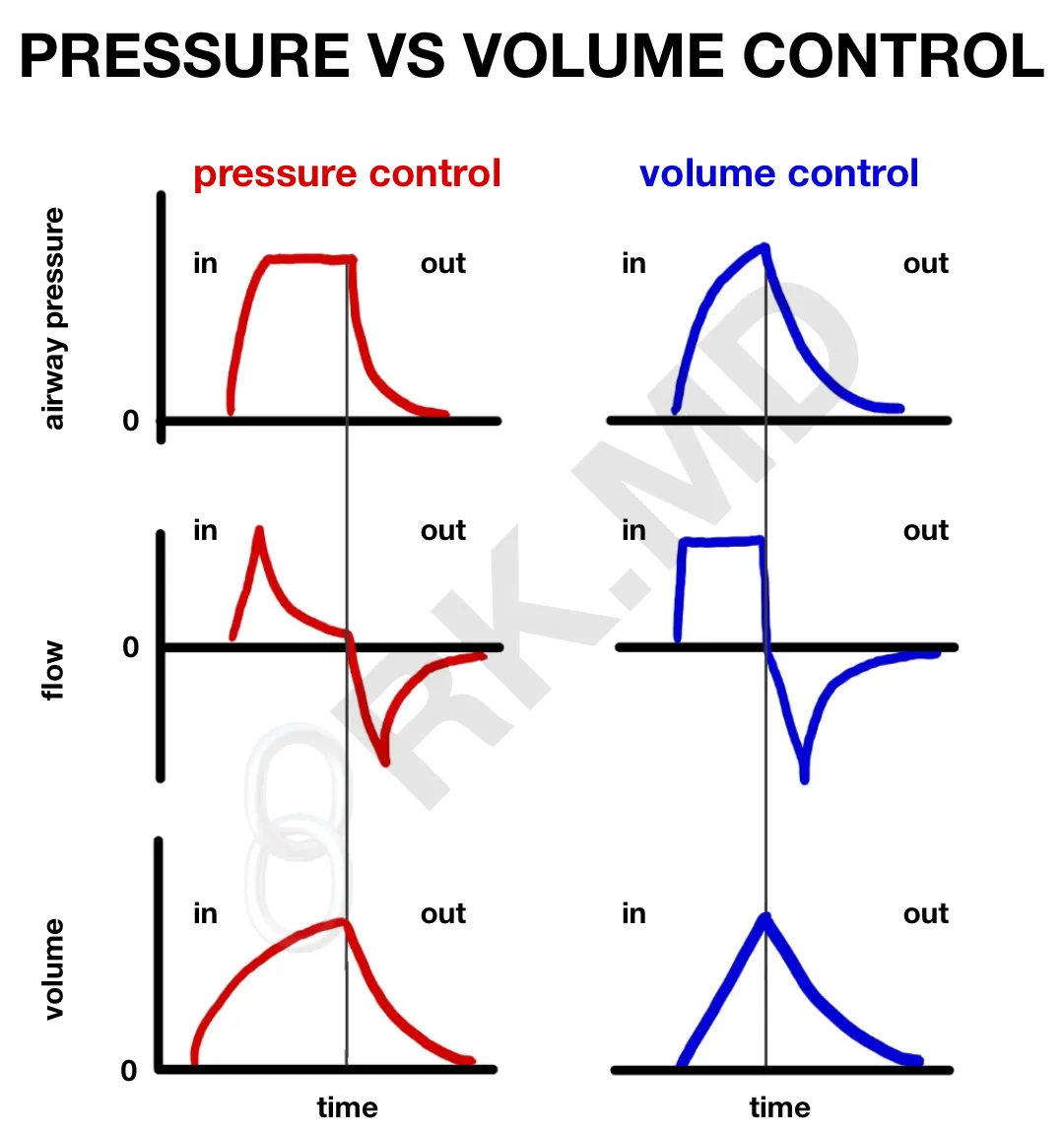
- Volume Control (A/C – VC)
- VT is directly set. Driving pressure will vary depending on the compliance although a “maximum” pressure can be set to avoid barotrauma.
- PEEP, FiO₂, and RR can be adjusted.
- A patient-triggered breath will result in the full VT being received.
- Flow is traditionally constant and maintained until the VT has been reached (“square waveform”). A decelerating flow is seen in pressure-control, volume-guaranteed variants of A/C-VC (downsloping flow in the latter parts of inspiration). This decelerating flow pattern is also seen in pressure control ventilation (see below).
- Ventilator will cycle to expiration once VT is delivered.
- A fixed minute ventilation is guaranteed since both VT and RR are directly adjusted. To increase minute ventilation, I usually consider changing the RR first rather than increasing VT which can lead to alveolar overdistension (volutrauma).
- Pressure Control (A/C – PC)
- Inspiratory pressure is directly set. VT will vary depending on lung compliance. For this reason, as the compliance changes (resolving pulmonary edema, worsening ARDS, etc.), the VT will change unless the inspiratory pressure is adjusted. Keep this in mind for any mode of ventilation where the inspiratory pressure is independently controlled.I/E ratio determines the amount of time spent in each phase (see the above explanation).
- PEEP, FiO₂, and RR can be adjusted.
- Usually cap the peak airway pressure around 30 cm H2O.
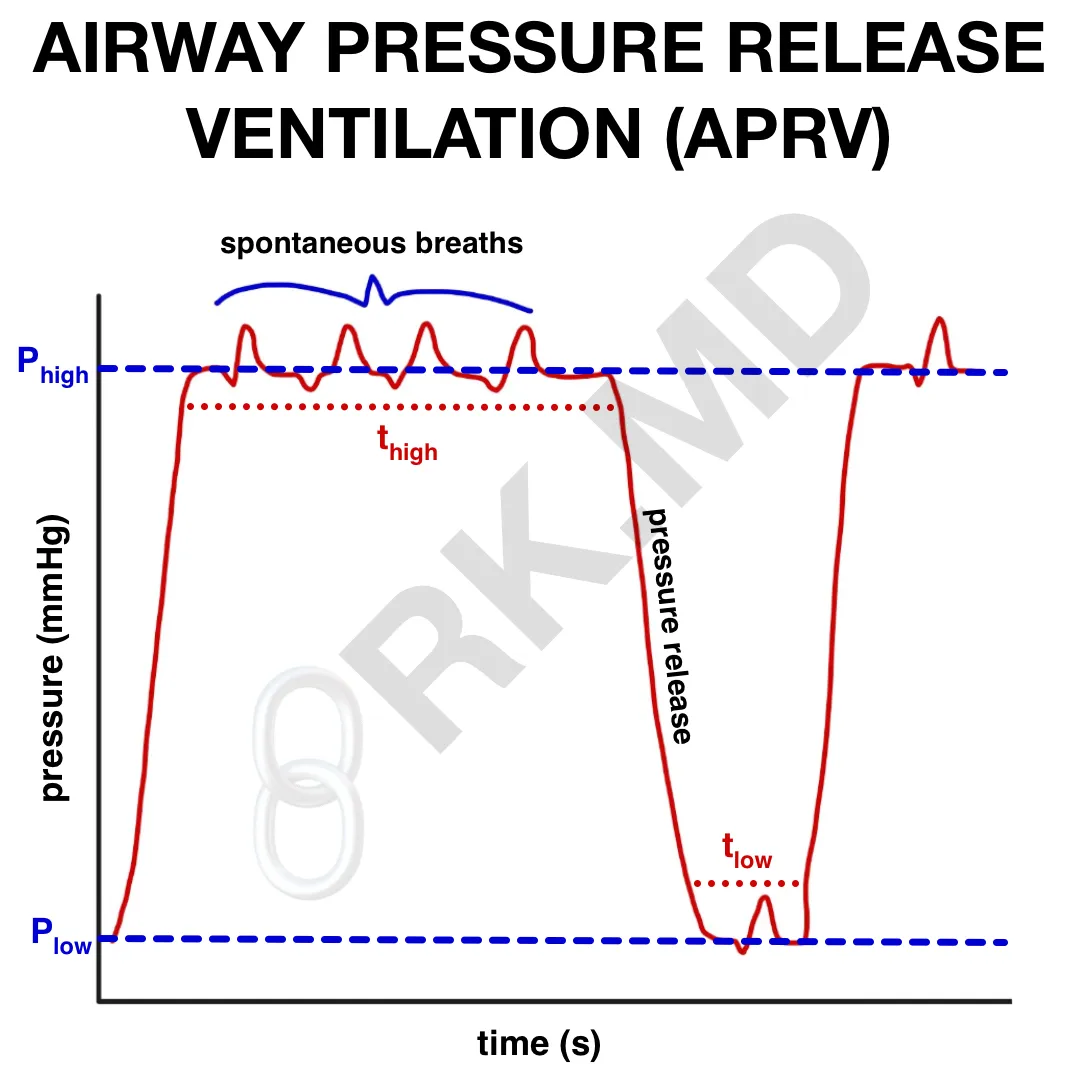
AIRWAY PRESSURE RELEASE VENTILATION (APRV)
Airway pressure release ventilation (APRV) is a pressure-controlled mode of ventilation that I sometimes try when I struggle with hypoxemia, such as ARDS or COVID pneumonia. APRV aims to improve alveolar lung recruitment by maintaining airway pressure at designated “high” (Phigh) and “low” (Plow) pressures for a set amount of time (Thigh and Tlow). This creates auto-PEEP to improve oxygenation. Think of breathing on top of CPAP with intermittent releases of airway pressure – that’s APRV!
When changing someone from a more conventional A/C-VC mode to APRV, I determine the plateau pressure and use that as my Phigh. Typically I start with a Phigh at 25 cm H2O and Plow at 0 cm H2O. Then, I start the time spent at the high pressure (Thigh) and the low pressure (Tlow) to 4 seconds and 0.5 seconds, respectively. By keeping the Thigh >> Tlow, the lungs don’t have enough time to depressurize completely, so the alveoli stay recruited. Also, since a complete breath takes Thigh + Tlow seconds, it makes sense that 60 / (Thigh + Tlow) is equal to the release rate (the “respiratory rate” on APRV).
Exhalation occurs after the airway is suddenly decompressed upon cycling to the Plow. The time spent at this low pressure (Tlow) is often difficult to gauge. Too short, and not enough air is exhaled, leading to decreased minute ventilation. Too long, and one runs the risk of extensive alveolar derecruitment. Finally, remember that APRV is an open lung ventilation mode, meaning patients can initiate their breaths at any point.
Weaning from APRV (essentially a CPAP mode) is accomplished by progressively decreasing the Phigh and increasing the Thigh time. Once the Phigh reaches 10-15 cm H2O, I’ll switch to a more traditional weaning mode (i.e., pressure support).
In summary, one can increase the FiO₂ and/or the mean airway pressure to improve oxygenation by increasing Phigh and/or Plow. In addition, ventilation is affected by the release rate and can be improved by increasing the gradient between Phigh and Plow, decreasing the Thigh time, or increasing the Tlow time.
SYNCHRONIZED INTERMITTENT MANDATORY VENTILATION (SIMV)
Although SIMV delivers a preset minimum number of breaths per minute, it “synchronizes” itself with spontaneous breathing initiated by the patient to avoid providing a breath as the patient is expiring. The mode of delivery can be anything (volume control, pressure control, hybrid modes).
The critical difference between A/C and SIMV is how they handle spontaneous efforts made by the patient. If the patient triggers the ventilator while on A/C, they will receive a fully supported breath (i.e., the full VT in volume control). In SIMV, they get whatever VT they can pull with predetermined pressure support from the ventilator. To a large extent, the tidal volume from a spontaneous breath is based on the patient’s respiratory strength and pulmonary compliance. If the patient is over-breathing their preset SIMV rate (i.e., VT of 450 ccs at a rate of 10 bpm), their VT can vary tremendously as the ventilator fully delivers some breaths and others are unsupported spontaneous efforts.
PRESSURE SUPPORT VENTILATION (PSV)
PSV provides just that – pressure support – with each breath spontaneously triggered by the patient who might be too weak on their own (i.e., respiratory weakness, emerging from anesthesia, etc.) In this mode, FiO₂, PEEP, inspiratory pressure, and a backup rate can be directly set. Remember that in SIMV, these same breaths would be unassisted. Like A/C – PC, the actual delivered VT depends on the patient’s pulmonary compliance. With changing compliance, this can lead to hypo/hyperventilation. Volume support ventilation (VSV) aims to solve this by automatically scaling the patient’s amount of pressure support to achieve the preset VT.
In either case, compliance should improve as respiratory strength recovers and/or pulmonary pathologies improve (less pressure to deliver more VT). For example, patients may need 15 cm H2O or more inspiratory pressure at the end of a long anesthetic to maintain a decent VT. However, after volatile agents have been weaned down and neuromuscular relaxation has been reversed, they may only need 5-10 cm H2O to achieve the same VT.
OTHER LINKS
Check out the following posts I’ve written dealing with pulmonology and mechanical ventilation:
- How We Breath – The Role Of Pressure Gradients
- Hypoxic Pulmonary Vasoconstriction (HPV)
- Bronchopulmonary Segments
- Functional Residual Capacity (FRC) And Pulmonary Vascular Resistance
- Work Of Breathing – Pressure-Volume Curve Integration
- Equal Pressure Point In Lung Physiology
- Interpreting Capnograms
- Automatic Tube Compensation (ATC)
- Extubation Criteria And Failure






When the covid Pt is places on a vent., and still failing , is the last resort v-v ECMO and in your opinion how effective is it? Or does it prolong the inevitable in those pts. whose outcome is already grim, giving them one last chance for survival?
3/1/2020 1605pm, Dr Kumar, What is the cheapest ventilator available that could be used to save lives in a mass Corona
Virus epidemic? What company makes it? How fast can manufacturers ramp up production of these ventilators? Should we petition Bill Gates Foundation and other great philanthropists to help us jump start creation of Ventilation Centers
where our citizens’ lives can be saved during the Corona Virus epidemic?
Thanks and can we keep in touch as this epidemic progresses?
You have a heck of a web site.
Yours,
Jerome I. Block, MD, MPH (Retired)
Certified, American Boards of Internal Medicine and Anesthesiology
I honestly don’t know, but it’s safe to say that we have no where near enough ventilators (or healthcare personnel) for a mass pandemic.
I’m a third year medical student. Just wanted to share with you that I do read your posts and you answer so many questions that I already had very succinctly and well. Many of these things are on my “to-read-more-about” list but, as you surely know, that list gets so lengthy. I really appreciate the posts! Keep at it.
You are very welcome! Glad you found the posts helpful! 🙂